Many thanks to Cheryl Strutt for this lovely blog about how she developed and used an Aromatherapy Talking Mat with people with learning disability.
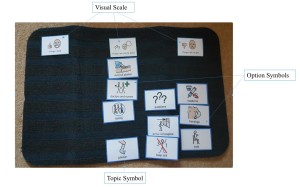
I am an Aromatherapist who works with adults who have a learning disability and often additional communication difficulties. As part of a recent service review I wanted to develop patient involvement. Talking Mats (TM) was suggested as a possible option to support patient feedback. I decided to look into this tool further and access training. During my TMs training I was supported to develop my specific Aromatherapy TM. The main aim behind this initiative was to adopt a system that could identify how each patient felt about the service and identify if there were areas where changes or improvements could be made. I wanted to work closely, alongside each patient, in order to learn how they really felt about their Aromatherapy treatments, their likes/dislikes etc. and to give them a sense of ownership of their sessions. It’s all about giving individuals with a communication difficulty a voice that can be heard.
The Aromatherapy TM supported patients to understand what is involved in an aromatherapy session and has been effective in helping them to personalise their session.
I used the Aromatherapy TM within the patient’s first session and following their last session, taking a photograph of the completed mats as evidence. The TM is an excellent way of offering a range of different types of massage experience and the patient can select their preferences. I found it an excellent way, to obtain valuable feedback on patient experience. One patient with a severe learning disability and autism was able through the use of symbols, to indicate his dislike for the music being played during his Aromatherapy session. He has no verbal means of communication and feedback like this would not have been achieved if the Aromatherapy TM wasn’t used. Through the implementation of the TM I now have evidence of patient centred practice, in relation to the therapeutic value of the Aromatherapy Service. The Aromatherapy TM supported patients to understand what is involved in an aromatherapy session and has been effective in helping them to personalise their session.
Since the implementation of the Aromatherapy TM, patient feedback is now at the heart of the Service. The patient is now able to openly give comments, make choices on their treatment plan, which in turn is making their attendance at the department, a very pleasurable one and it’s very personal to the individual. Another patient who said that he wasn’t able to read or write, was able to explain what the symbols meant and chose the symbol for happy. He went on to indicate his preferences stating ‘I like foot-spa and a foot massage.’ Prior to using the TMs, I was often reliant on observing the patient’s body language to assess their level of enjoyment and gain feedback. The Aromatherapy TM now allows for a more accurate method of evaluating interventions. I am so enthusiastic about the increased level of patient involvement and the willingness of the patients to become involved in this activity. This project clearly demonstrates the value of involvement, leading to improved partnership working and better experiences.
Cheryl Strutt, Aromatherapist, Cheryl.strutt@belfasttrust.hscni.net
We are very grateful to Mary Walsh, Senior Speech and Language Therapist at St Mary’s Hospital in Dublin, for her Blog ;Does he like fairy cakes? ‘ It has been taken from her report on a project which looked at how speech and language therapists can facilitate the involvement of people with dementia to become more active participants in the decision making process around dysphagia management at the end stage of dementia. The project was funded by the Irish Hospice Foundation Changing Minds Programme
The project aims were:
- To improve person centred care in relation to residents’ food and drink preferences and dislikes
- To actively involve the residents of the dementia specific unit in the decision making process around their dysphagia (swallowing) management particularly at the end stage of their lives.
In order to find out the food and drink preferences and dislikes of the residents, the team carried out staff questionnaires and family questionnaires. They found that, although these were useful in getting a quick overview, there were a lot of unanswered questions.
The team also used Talking Mats and found it to be a powerful way to explore the residents’ food and drinks preferences and dislikes when used with suitable candidates. Participants appeared to really enjoy the experience including looking at pictures of the completed mats afterwards. This may be because they felt heard, that their views mattered and/or that they felt empowered. The information was important for current Dysphagia management, and also as an advanced directive in the documented evidence of the residents’ wishes in the recorded pictures of completed mats.
Brief Case Study: Does he like fairy cakes?
Talking Mats was used with a gentleman who may have been assumed to be unsuitable to use Talking Mats as he was assessed as having late stage dementia. However, this man engaged readily in the Talking Mats interview and appeared to be happy to have his views recorded. Also, there was a much higher level of correlation than variance with Talking Mats and both the staff questionnaire and the family questionnaire thus further indicating that he was a suitable candidate. ‘Fairy cakes’ was something that this resident reportedly liked in both the staff questionnaire and the family questionnaire. However, the gentleman indicated twice on Talking Mats that he disliked fairy cakes.
A number of actions are proposed in the report including :
- Continue to use Talking Mats as appropriate in the dementia specific residential unit and the rehabilitation wards of St. Mary’s Hospital.
- Inform the multi-disciplinary team of the merits of Talking Mats. This tool can also be used to explore other important issues for suitable residents/ patients on a case by case basis.
Conclusion:
It is essential to challenge our assumptions in our dealings with people with dementia. Truly person centred care takes time and patience where assumptions are challenged. Also, it is essential to listen to what residents tell us verbally, or through a supported communication system such as Talking Mats or non-verbally through tone of voice, facial expressions or gestures, and to act according to what is being communicated.
Many thanks to Greg Cigan for this great blog about his study that explored how children and young people with an intellectual disability feel about undergoing clinical procedures.
A clinical procedure is any activity performed by a healthcare practitioner to diagnose, monitor and/or treat an illness such as blood pressure testing, x-rays and other scans (Cigan et al., 2016). While some procedures cause no pain or only mild discomfort when completed, others can be prolonged and potentially painful (Coyne and Scott, 2014). Children and young people with an intellectual disability are more likely to develop physical illnesses including epilepsy and digestive disorders than the general population and can be frequently required to undergo healthcare procedures (Emerson et al., 2011; Short and Calder, 2013). Yet, there is currently little empirical research reporting how children and young people with an intellectual disability experience procedures (Peninsula Cerebra Research Unit, 2016). More research is required so that healthcare services can better understand the needs of children and young people with an intellectual disability (Oulton et al., 2016). As part of my doctoral studies at Edge Hill University, I am conducting a study that explores how children and young people with an intellectual disability experience having a clinical procedure.
From the outset of the study, I felt it was important to obtain data directly from children and young people rather than relying on parents and carers to speak on their behalf. I was keen to adopt methods during interviews that would enable as many children and young people as possible to take part, including those who find verbal communication challenging. After researching different methods, I chose to utilise Talking Mats as the innovative design of the tool offered children and young people the option to express their views entirely non-verbally should they wish to by arranging symbol cards. To date, I have interviewed 11 children and young people about their experiences of undergoing procedures. Each participant was between 7-15 years of age at the time of the interview and had a mild to moderate intellectual disability.
Prior to an interview beginning, I spent time describing and showing each child/young person a Talking Mat and asked whether they would like to use the tool during their interview. Out of the 11 children and young people I have interviewed, three used a Talking Mat. Those that chose not to use the tool were older children who were confident having a verbal conversation with me or those who had a visual disability and could not see the symbols. In all cases, the decision of the child/young person in relation to using the Talking Mats was respected.
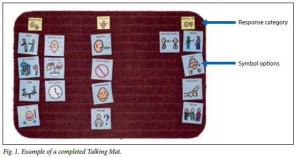
The three children who used the Talking Mats were able to express their views non-verbally and also seemed to convey more information than some of those who chose not to use the tool. Viewing the symbol cards within a Talking Mat appeared to help children and young people break down information into smaller chunks which then made it easier for them to process and discuss. Indeed, using a Talking Mat led all three children to discuss information that was new to their parents who sat in while s/he was being interviewed. An example of a completed Talking Mat is shown below which was created by an 11-year-old boy during his interview. The boy clearly expressed that he did not enjoy his experience of having a clinical procedure.
Within my study, I feel using Talking Mats has helped to augment the verbal communication of some of the children and young people which in turn enabled them to take part in interviews and share their views and experiences of procedures. Talking Mats are a valuable tool for researchers working within the field of intellectual disabilities. If used more widely, Talking Mats has the potential to enable more children and young people with intellectual disabilities to have the opportunity to be involved and express their views within healthcare research.
Reference List
CIGAN, G., BRAY, L., JACK, B. A. and KAEHNE, A., 2016. “It Was Kind of Scary”: The Experiences of Children and Young People with an Intellectual Disability of Undergoing Clinical Procedures in Healthcare Settings. Poster Presented at the 16th Seattle Club Conference (Awarded Best Poster Prize), 12-13 December. Glasgow: Glasgow Caledonian University.
COYNE, I. and SCOTT, P., 2014. Alternatives to Restraining Children for Clinical Procedures. Nursing Children and Young People, 26(2), pp. 22-27.
EMERSON, E., BAINES, S., ALLERTON, L. and WELCH, V., 2011. Health Inequalities and People with Learning Disabilities in the UK: 2011. Lancaster: Improving Health and Lives: Learning Disabilities Observatory.
PENINSULA CEREBRA RESEARCH UNIT, 2016. What’s the Evidence? Reducing Distress & Improving Cooperation with Invasive Medical Procedures for Children with Neurodisability. Exeter: University of Exeter.
SHORT, J. A. and CALDER, A., 2013. Anaesthesia for Children with Special Needs, Including Autistic Spectrum Disorder. Continuing Education in Anaesthesia, Critical Care & Pain, 13(4), pp. 107-112.
If you would like more information about Greg’s work you can contact him at Cigang@edgehill.ac.uk
Many thanks to Shirley Rush Health Facilitator at Belfast Health and Social Care Trust for this great blog about using TM as a ‘weigh to health’.
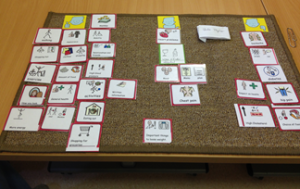
Following my Talking Mats (TM) training I had the opportunity, as a health facilitator, to use TM in an adapted ‘Weigh to Health’ course. This course encouraged people with learning disabilities to make small changes to their lifestyle and to educate them on the effects of obesity and their health.
Prior to commencing the group work we met with each person and completed a Talking Mat. The topic was to explore “Important things to lose weight”, we used a wide range of symbols and included physical activity, health conditions and appearance. Clients also requested additional symbols were added including alcohol, cycling and mood, which made the mat individual to them.
A photograph was taken of the completed TM to act as a record of what was important to them. On completion of the group the TM was repeated with each person using the same topic and symbols and the mat was again photographed. When we compared the TMs it showed that all the client’s knowledge and understanding of the effects of obesity and the health benefits associated with weight loss had increased.
“it done me good, helped me to lose weight by talking about my health and the need to lose weight to look after my heart”
The use of the talking mat was a valuable resource, it allowed each client to make an informed choice about participating in the group work. One client said he felt he had been listened too and “it done me good, helped me to lose weight by talking about my health and the need to lose weight to look after my heart”. By using TM in this way we have been able to use this information to demonstrate outcomes and it shows the information was presented at a level of understanding suitable for the client group. On an easy read questionnaire about the course all the clients agreed that doing the TM was useful, one person wrote “loved doing the mat”.
If you want to get more information from Shirley contact her at Shirley.rush@belfasttrust.hscni.ne
Talking Mat would like to wish you all a Happy Christmas
2106 has certainly been a busy year for us at Talking Mats. We have seen some staff changes saying goodbye to Jill hall and welcoming Morag Crawford. We were delighted when we brought Kirsty onto our staff . Kirsty originally volunteered with us as part of a school transition programme for people with autism. Laura Holmes joined us as a Talking Mats external associate for the North West of England.
If you are interested in what we do and want to see our activity in numbers then have a look at the Talking Mats Year in numbers . Click on image to see the enlarge !
At the moment we are busy preparing for 2017 and we are looking forward to
- The evaluation of our following projects in The New Year
- The National Involvement Network on our partnership with ARC Scotland
- Our programme of service wide training with Central London Community health
2 Continuing to work with
- Patient Opinion
- The Alliance Self-management digital project
- Colleagues in Germany
3 Launching more resources
- Keeping Safe- so far this resource has only been available to people working with people with learning disability in Scotland. We will be holding a specialist seminar about this resource in London on the 17th March so its use can extend south of the border .
- Launching our conversation sets: gardens, holidays, trips out, sports indoor, sports outdoor and football. These were developed as part of the family training for people with dementia but they have much wider use and will be available as additional Talking mats sets
Plus Talking Mat is planning to go to Australia in May!
Nicki and Lois have their flights booked. Agosci here we come ! Then we are over to New Zealand to run foundation training in Christchurch and Auckland before we head back to Melbourne to run the first ever accredited training course in Australia. We will also be running a specialist seminar on Keeping Safe in Melbourne. If you want any details about the trip please get in touch.
We really appreciate all the support we get from everyone involved in Talking Mats and wish you all a happy and peaceful festive season
We have received a number of requests to create a guide to adding your own images and creating submats with Digital Talking Mats and this blog will show you how.
One of the features of Talking Mats is that we have developed a number of different symbol resources based on our research and clinical practice which cover a wide range of topics.
However, sometimes you may want to personalise what is being communicated about by adding your own images. You may also want to create a submat to explore an existing topic in more detail or you may want to create a completely new topic. In our training courses we explain how to do this when using the original Talking Mats.
However more and more people are now using the digital version of Talking Mats. In a previous blog we described how to add your own photos to the Digital Talking Mats.
We have now made a guide to help those who have the digital version to both add their own images and to create a submat with an example of a sub-mat with the topic “office”.
Download the following pdf to find out how to do it. dtm-a-guide-how-to-add-photos
We would love to hear any stories about making your own digital submats
This blog describes the foundation Talking Mats course we ran for members of the National Involvement Network. Following the seminars and the work to design a Charter for Involvement ‘Taking Part Talking Mat’ described in a previous blog , 16 people attended our course run over three days with about a month between each session. The participants were 8 NIN members who all had a worker to support them as a learning partner. Their role was to assist with embedding the knowledge gained, and the implementation of the pilot ‘Taking Part Talking Mat’. The learning partners were equal course participants, and expected to complete all course activities e.g. make a video of themselves carrying out a Talking Mat
In adapting the foundation Talking Mats course we learnt lots! Here is a summary of key learning.
- That we had a great group of people who were keen to learn and develop their communication practice to become Talking Mats interviewers, or as we call them in Talking Mats ‘the listener’ ( as they are listening to someone’s views). They appeared to really enjoy the learning experience and were enthusiastic, embracing all tasks including making a video of themselves using Talking Mats with someone in their organisation. In Talking Mats we call the person doing the mat ‘the thinker’.
- That it was really important for us as trainers to focus on key information, not all information so as not to overload
- That movement helped learning. It was good to design activities with some potential for movement so that people were not sitting too long and that they could get up and stretch.
For example, on the Talking Mats foundation course there is an activity that thinks about abstract and concrete language. We adapted this by using cut out coloured circles and got participants to think about the language load of a particular concept and place the symbol concept in the relevant circle.
- Teaching the principles of Talking Mats and getting the participants to follow the rules e.g asking open questions, introducing blanks, the check and change stage was relatively easy. What was more problematic was supporting a listener to be flexible and person centred in the way they introduced an concept . Often it is important to give a relevant example to support a thinker’s understanding and our listeners struggled with that. To overcome this, we wrote specific examples on the back of the cards and designed some activities to give time to practice. Repetition of learning was important
- A detailed script helped, including what to say to introduce the Talking Mat
- That you needed to pay particular attention to the quieter members of the group –coffee breaks proved to be a useful time to catch up on their thoughts and feelings
- The role of the learning partner is critical. We were very fortunate in our partners. They were natural enablers and it showed. We relied on partners sharing a set of values, and believing that people with learning disabilities could learn and be a key member of the pilot project.. One person did not complete the project maybe because she felt uncomfortable. It made us realise if we were to do this again we should be explicit about values and the roles of the learning partner from the outset
- That the recording of interviews needs support, and it was key that there were was both a NIN member and a learning partner to enable that to happen
- That our partnership with ARC Scotland was key as they provided individual follow up advice to each of the organisations involved and provided a source of learning reinforcement , observation and support to each of the NIN members and their learning partner. They were also able to feedback to the course organisers about any areas of difficulty that needed further attention and input
- That Talking Mats empowers both the thinker and the listener. It gives a structure to make a conversation flow. The training itself not only gave the NIN members who attended a tool to communicate with others about how they feel, but also seems to have had a positive knock on effect on their confidence and we hope that continues.
We are incredibly proud of our cohort of trained Talking Mats listeners. As part of the project they have been interviewing other service users in their organisations about 2 aspects of the Charter for Involvement –‘independence’ and ‘being involved in their community’ – ( 2 abstract concepts, as the NIN listeners will tell you). Not only has this included more people in service evaluation but has led to making changes that are improving lives.
For example
One woman was no longer being taken to church and she is now going and starting to be part of a local church community
One man who everyone thought was doing really well living on his own expressed a view that he was feeling lonely, He is now being supported to identify if there are enough people interested to start a local group.
Two videos were made by the group the first shows what they found out using their Talking Mats tool
Exploring sibling attitudes towards participation when the younger sibling has a severe speech and language disability
We were delighted to receive this publication from a friend and colleague, Prof Juan Bornman from Pretoria in South Africa. It reports on a study carried out with 27 typically developing children who have a younger sibling with a severe speech and language disability. Juan and her colleagues used Talking Mats to carried out an adapted structured interview to find out the views of these children on four everyday life situations identified by the WHO-ICF-CY (World Health Organisation’s International Classification of Functioning, Disability and Health, Children and Youth Version).
The four topics were:
Communication
Domestic life
Interpersonal interaction and relationships
Major life areas.
The findings showed that the children were ‘most positive towards participation in play activities with their sibling with a disability. They were also positive towards participation in household tasks. They were less positive towards communication participation and least positive about participation in interpersonal relationships’.
The following example is taken from Juan’s publication.
The article’s reference is:
Exploring sibling attitudes towards participation when the younger sibling has a severe speech and language disability. M Hansen, M Harty, J Bornman South African Journal of Child Health 2016 Vol. 10 No. 1
To read the full publication with details of the methods used and the results click here sibling-attitudes-2016
Delighted to introduce you to ‘The Communication Game’ : a board game for staff to improve their communication skills.
How we listen, talk and engage with people is fundamental to the quality and effectiveness of health and social care services. Although communication underpins everything we do in a work context, it can be a difficult topic for staff to talk easily about. Add to that the possibility of service users having an additional communication support need, through reasons like stroke, learning disability or dementia, then there is much potential for things to go awry and unfortunately, they often do. ‘Poor communication’ is cited as the most common cause of frustration in complaints about services.
The Communication Game was developed by Focus Games, NHS Education for Scotland (NES) and Talking Mats. It is a learning tool to help staff working in the health & social care sector increase their knowledge and skills around communication. The Communication Game is fun and easy to play. It can be played with or without a facilitator, and allows staff groups to have discussions and reflect on their communication skills. It allows them the chance to learn from each other. It will improve knowledge, but more importantly enable them to think about the small steps they can make to improve their interactions.
The project grew out of two previous projects funded by NES: Making Communication Even Better and Through a Different Door. In these projects, it was recognised that the experience of services for people with a communication support need is something of a lottery. For them, there was a considerable difference in the experience of interacting with a staff member who was empathetic and able adapt to their communication, to interacting with a member of staff who was struggling and unable to adapt their interaction. Training and understanding of inclusive communication practice is key. It has been a great privilege for Talking Mats to continue to support the work of the previous 2 projects and work with Focus Games Ltd to develop The Communication Game. Support during the development process from the Stroke Association Scotland, Capability Scotland, RCSLT, Scottish Care, Communication Forum, Queen Margaret University and NHS Ayrshire & Arran SLT Department have been invaluable, and we are very grateful; also to NHS Education for Scotland for their continued input and funding.
If you are working with staff in the health and social care sector, then this will be a great resource for you. You can get The Communication Game from the Focus Games online shop. It is guaranteed to promote laughter learning, and a touch of competitive team spirit. Most importantly, it will be a catalyst to help develop staff communication, making interactions better for people with communication support needs.
You can find out more about the game at www.communicationgame.co.uk
, and follow the game on Twitter on @Comm_Game.
Get your copy at www.focusgames.com.
Many thanks to Ruth Spilman, Senior Speech and Language Therapist, for this great blog about how she uses Talking Mats for Capacity Assessments with People with ASD/LD
I am a speech and language therapist (SLT) working in a residential provision for young people with autism spectrum disorder, learning disabilities and other co-occurring difficulties. We support young people from 7 up to the age of 20. Many of the young people are in a ‘grey area’ with a view to capacity assessments, including those aged 16-18. We support many capacity assessments, including deputy-ship for finances and care, health and welfare, as well as more individualised capacity assessments around restrictions in the environment, consent to medical interventions and making decisions about the future.
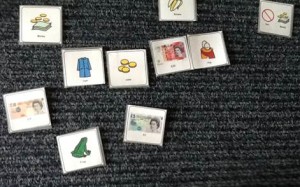
A large part of the way we support these capacity assessments is by using Talking Mats, which support people with autism who generally prefer to think about things visually. The young people are encouraged to use Talking Mats in their everyday communication, such as evaluating activities, lessons and therapy sessions to develop their skills, as well as during direct Speech and Language Therapy work. If a young person has proven their competence using a Talking Mat, we can then move on to supporting capacity assessments. As part of the process, the SLT would break down the concepts needed to be understood to identify if the individual has capacity or not. For example with finances, do they know what money is? can they organise things that are expensive and cheap? can they put items in a scale of least to most expensive? This would all be done using a Talking Mat, then followed up if they achieved this task with a range of further activities. A Talking Mat can then support activities to evidence their understanding or lack of, while also giving a young person all practicable help to communicate.
See below two examples of a young person thinking about 1) money to support their finances, and 2) things that are healthy or not.
Talking mats are used for a range of different skills and assessments in the provision I work in, but their use for capacity assessment gives the young people the most practicable support with communication and allows for clear evidence of the person’s understanding of the concepts involved. In addition to the range of items mentioned above, we have have also discussed tattoos, physical intervention and behaviour support strategies, having a lock on an individual’s bedroom door, and understanding of fantasy and reality.
Talking Mats has proved to be a truly simple but brilliant and useful tool.
Ruth Spilman, Senior Speech and Language Therapist, Specialist services in education
The Cambian Group, Dorset, BH19 1PR www.cambiangroup.com
 Online training login
Online training login