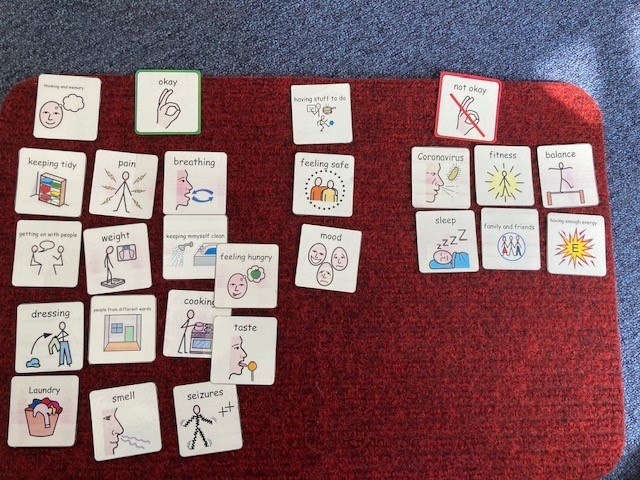
As a group of Allied Health Professionals (AHPs) working in a secure hospital we recently embarked on a mini project using Talking Mats to check in with our service users with learning disabilities during Covid-19. We collated the evidence from our respective professional bodies (Royal College of Occupational Therapy, Royal College of Speech and Language Therapy, Chartered Society of Physiotherapists and British Dietetic Association) in terms of changes that people might experience if they’d had Covid-19 and produced a talking mat around these.
It quickly dawned on us that we might be on to something here, and that creating an opportunity to ‘check in’ more broadly with our service users would serve a useful purpose, so we added some additional categories around changes to routine, psychological wellbeing and feeling safe.
This was my colleagues’ first experience of using talking mats, and their faces when I turned up clutching my 99p actual doormat were a picture! I introduced them to the theory behind the mat and its presentation and harped on about the benefits in terms of attention, comprehension, non-threatening interaction, initiation and structuring narrative; they nodded supportively.
We set off across our learning disability wards in multi-disciplinary pairs and all but a few of the service users agreed to have a chat with us. My colleagues commented that they were pleasantly surprised by the engagement and the amount and novelty of the information gained; we identified things that the service users hadn’t told anyone because they hadn’t been asked that question!
In talking to others we were asked why weren’t rolling this out in a partner secure hospital for people with mental health conditions? ‘no reason really, we just haven’t got there yet’ we answered. Then came the…. but we can just do it like a questionnaire with them. This question wasn’t, and in my experience isn’t ever ill meant. It comes from a place of naivety in relation to the presence of communication difficulties in people with mental health conditions and because of that, lack of exposure to different professional groups such as Speech and Language Therapy and the skills and approaches we have to offer. Skills in gaining and holding someone’s attention. Skills in decreasing pressure in communication situations. Skills in enabling time, space and ways in which people can initiate their thoughts.
The Multi-Disciplinary Team (MDT) working around the project has enabled me to show others how talking mats can support their practice. It has enabled them to see how a very simple and non-threatening visual tool can open up conversations and lead to information that the service users hadn’t shared before, in a way that a face to face conversation doesn’t.
Thanks to Jo Brackley, Clinical Lead, Speech and Language Therapy Secure Services at Cumbria, Northumberland Tyne and Wear NHS Foundation Trust for this inspiring blog – which demonstrates when we shift the way we listen and gather information from patients we get a different result and improve the quality of information and communication . If you or your team want to consider Talking Mats training then we can provide this for organisations . At the moment we can take a cohort through our online course together and then arrange a zoom call to discuss application to your work setting – email info@talkingmats.com for more information.
In our latest blog, Rachel Woolcomb, Talking Mats OT Associate, discusses how Talking Mats can support Reflective Practice for Occupational Therapists.
Taking time out to stop and reflect on our practice can be a challenge. We convince ourselves there are more important things to do, people to see, targets to meet, and therefore we just don’t have the time.
However, I suggest, that with this mind set we are doing ourselves, and the people to whom we provide support and care, a disservice.
Clinical supervision has always been embedded in the culture of occupational therapy and at its best should create a safe and supportive environment in which reflective practice can take place.
Unfortunately, in practice, the reality can look different.
The more I have used Talking Mats to enable my clients to think and express their opinions, the more I have been convinced, that there is also great benefit to them being used within the clinical supervision process.
I want to thank the occupational therapists who agreed to explore this further with me. They used Talking Mats to think about their coping skills at work, or reflected on how their ability to learn and think, impacted their job role.
They were surprised how easy they found it to think about the full breadth of their working life and the impact this had on their wellbeing. As clinicians, we are great at looking after other people and ensuring that their health and wellbeing needs are met, however, we are not so great at caring for ourselves.
The latest TMOT resource provides more information about why and how, Talking Mats can be an effective tool in enabling a reflective thinking space for clinicians. Check it out here: TMOT3 Reflective practice
Give it a go… You are worth it!
To find out more about our Talking Mats resources, check out this link:
https://www.talkingmats.com/shop/
In this latest blog, our Talking Mats OT Associate, Rachel Woolcomb tells us how Talking Mats can support delivery of Personalised Care:
“Person centred practice”, and “partnership approach” are common phrases heard in health and social care settings but what does this really mean in practice?
How good are we at ensuring our service users are truly heard, and given opportunities to talk about what is important to them?
Recently NHS England set out their ambitions for the delivery of personalised care. This is a commitment to enabling people to have the same choice and control over their mental and physical health that they have come to expect in every other part of their life.
This however requires a shift in culture.
One of the cornerstones of personalised care is shared decision making. This is a collaborative process in which people are supported to understand the options available to them including the various risks, benefits and consequences. A shared decision will have acknowledged personal preferences, circumstances, values and beliefs. This ensures that when a choice is made it is fully informed.
There is substantial literature which demonstrates the usefulness of goal setting as part of the communication and decision making process.
A well written person-centred goal will describe the anticipated achievement of a specific activity. It will be meaningful and help create a common vision within the rehabilitation process.
Talking Mats is an ideal tool to help facilitate these processes. They enable better conversations and provide an interactive thinking space. They have also been demonstrated to be a useful tool in enabling people to think about their rehabilitation goals.
Read more about this in the TMOT Resource 2: How Talking Mats can help facilitate shared decision making and goal setting: Goal setting TMOT 2
If you would like to find out more about the different Talking Mats training options we offer, take a look here: https://www.talkingmats.com/training/
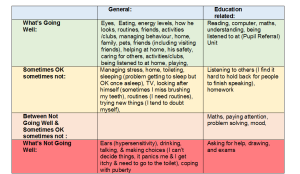
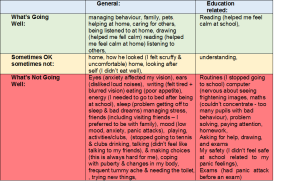
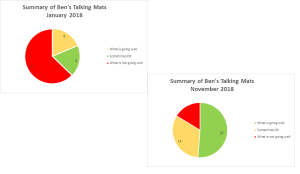
Many thanks to Tina Wood, Occupational Therapist at Therapy In Motion, for this great example of how Talking Mats can be used to explore thoughts and feelings both in present-day and in retrospect, to evidence positive outcomes from a change in educational placement. Tina’s use of colour coding and pie charts really helps to illustrate this.
Tina attended our Talking Mats Foundation training back in September 2016 and since then she has been using Talking Mats regularly in her work as an Independent Occupational Therapist.
In this example, Tina has used Talking Mats to enable Ben (name changed for anonymity, age 12½ years) to share his thoughts and feelings using the Talking Mats ‘Consulting Children and Young People’ resource packs – focusing on the topics ‘My Body and Skills’ and ‘What I do and Support’.
At the time of this Talking Mat, Ben had been accessing a new placement at a Pupil Referral Unit for the past 11 months (click on the picture below to see a clearer version).
As there was clearly a difference in how Ben felt things were going when he was attending his previous school, Tina decided to ask him to do a retrospective Talking Mat of how things were going for him 11 months ago in January 2018, when he started to feel “unwell”.
This enabled comparison with how he feels now in the “safe setting” of the Pupil Referral unit (click on picture to see a clearer version).
Tina then compiled the information from the above tables into pie charts, enabling a clear visual comparison between the two times/situations (click on picture to see a clearer version):
As can be seen from these charts, there had been a huge change in Ben’s perception of how he is coping with life in general and school in particular.
Tina recommended that this information needs to be considered along with the rest of Ben’s sensory needs (as reported in her full OT report) when deciding on what is the best educational setting for him after leaving the pupil referral unit.
We love this use of colour coding and pie charts to illustrate the information from Ben’s Talking Mats – to really ensure that Ben’s feelings and thoughts are seen and heard.
If you would like to know more about accessing Talking Mats training – available across the UK and Ireland as well as online – please take a look here: https://www.talkingmats.com/training/
If you have any examples of how you report/share information about completed Talking Mats we would be interested to hear about it! Just email laura@talkingmats.com
Rachel Woolcomb, our Talking Mats OT Associate, tells us about the recent Royal College of Occupational Therapists’ Report and considers the ways Talking Mats can support:
The Royal College of Occupational Therapists have recently published a new report. “Making personalised care a reality: The role of occupational therapy.”
As the OT Associate for Talking Mats, I took the opportunity to review the document and consider how Talking Mats can help OT’s in fulfilling the recommendations made.
The report recognises that people living with long-term conditions bring different and equally important, knowledge and expertise to the decision –making process.
It challenges OT’s to ensure that they really listen to, and hear the views of the people they work with.
A Talking Mat can help facilitate this. It helps people to understand what is being discussed, to reflect and organise their thoughts, to say what matters most to them and record their views. It helps OT’s to really listen, to learn new information, to involve the person in their own planning and support decision making.
Read more about how Talking Mats can help OT’s to make personalised care a reality in the TMOT Resource 1: TM Personalised Care – Copy.
The RCOT report is available here: https://www.rcot.co.uk/news/delivering-personalised-care-frontline
Rachel would love to hear from you if you have any examples of how Talking Mats have helped you to provide personalised care, or if you want to know more about OT and Talking Mats. Her email is: Rachel@talkingmats.com.
If you are feeling inspired and would like to find out about accessing Talking Mats Foundation Training, take a look at our upcoming courses across the UK, as well as online and organisational training options: https://www.talkingmats.com/training/
We are delighted to introduce Rachel Woolcomb our first Talking Mats OT Associate. She is joining the Talking Mats Team and will be working to develop awareness and use of Talking Mats by Occupational Therapists. I will let Rachel introduce herself:
I am delighted that Talking Mats have asked me to join their team for one day a week. I am passionate about occupational therapy and about Talking Mats and to have the opportunity to bring these two loves together and seeing what develops is very exciting.
I live in South Gloucestershire and have had a varied career since I qualified as an Occupational Therapist in 1992. I was introduced to Talking Mats in 2008 and have never looked back, using them with my clients ever since.
In 2017, having spent over 25 years working in the NHS, I made the decision to move into independent practice. I work predominately with teenagers and adults who live with long term neurological conditions or who have experienced catastrophic injuries following trauma. I am very aware of the psychological impact of sudden disability and the need for people to be able to express who they are and what is important to them, even in difficult circumstances.
I now use Talking Mats with most of my clients. It doesn’t matter if they are old or young, can speak or have communication needs, they all benefit from the opportunity to stop and think and have someone really listen to them.
In the last few weeks a man who has had a stroke and has limited expressive speech has used a Talking Mat to talk about what leisure activities he used to enjoy. He then used a second mat to explain what he can and cannot achieve now. This helped us together, set goals for occupational therapy. I am also working with a teenager who has had a traumatic brain injury and now struggles with her education. She uses Talking Mats with me regularly, to think about her coping skills at school. Looking back at her previous mats is helping her to recognise progress. I have so many more examples and will be sharing them with you soon!
I really want to inspire OT’s, helping them to consider how they enable their clients to think, communicate their choices and make decisions. A Talking Mat is a great for this. It is also creative and interactive something that in my experience OT’s like! I will also be looking at important issues within the field of occupational therapy that are currently driving practice, such as personalised care, goal setting and shared decision making. I believe it is vitally important that we collaborate with our clients as together we can achieve so much more. Talking Mats is an effective tool in enabling this, so watch this space, and please do get in touch if you want to know more or have stories to share.
It is great to have Rachel working with us to build on some of the excellent work being done already in the Occupational Therapy Sector. Our Director, Lois Cameron shares why we are so excited to welcome Rachel to our Team:
‘I am really pleased that Rachel is joining us . I think the Talking Mats approach sits well with the values and approach of Occupational therapy, In my experience OTs are naturally holistic in their approach. I remember at a training course in London an OT said for her Talking Mats was the missing link in her toolkit. The training and experience of OTs allow them to see things through a different lens and that will be really helpful to us’
For more information about how OT and Talking Mats are a winning combination, take a look at Rachel’s recent blog – https://www.talkingmats.com/talking-mats-and-ot-a-winning-combination/
Feeling inspired and want to know more about the training courses we offer? See www.talkingmats.com/training/ for details.
We are grateful to Rachel Woolcomb OT, for sharing this Talking mats story.
Within my occupational therapy practice I have found Talking Mats to be an excellent thinking tool to help my clients establish their priorities for therapy.
I was asked to work with a teenage girl who had sustained a brain injury resulting in a mild cognitive impairment which was impacting on her participation and ability to learn at school.
She had undergone formal cognitive testing with a clinical psychologist, however had shown poor levels of engagement with the assessment process (which had taken over two hours). She was reported as having erratic focus and inconsistent answers to questioning. The results were therefore deemed to be inconclusive and no recommendations made. I knew that Talking Mats would provide me with similar information to that which the psychologist was trying to gain, but in a way that would be engaging and client focused. I also felt that the concept of the Talking Mat, which enables the thinker to express their own views rather than a “right or wrong” answer, would help to improve participation.
I selected the learning and thinking topic cards from the communication set within the Health and Wellbeing pack. These cards cover areas that I would normally look at within any cognitive assessment and are functionally relevant. Together we selected the visual scale, choosing the question “how well are you managing?”
She explained that organising herself, writing, listening, reading, problem solving and planning were all going well. She talked about how she sometimes had difficulties concentrating and paying attention due to getting distracted in the classroom. She also felt she was struggling more than before with calculating and that this was affecting her scores in Math tests. She explained that remembering and making decisions were “not going well’ and she was particularly worried about the fact she had forgotten some of the teaching she had received prior to her brain injury. I was also able to conclude from the way she understood the concept of the mat, as well as her ability to engage and attend for the whole session, that she could concentrate, learn new skills and had the ability to weigh up information to help her make decisions.
Together we used the information gained from the Talking Mat to set goals for therapy which were focused around having a range of strategies to help her concentrate in class, remember new information, and make decisions.
Two months later, once having completed a therapy programme, we used the Talking Mat again to explore her current thinking about the topic area. She explained that making decisions was something she no longer had difficulty with as her confidence had grown. She felt that there had been some improvement with her ability to remember information and we discussed the strategies she now used to help her concentrate in class, which included ways to minimise any distractions.
In summary, the Talking Mat enabled her to think about how her brain injury had affected her ability to remember, make decisions and learn. This provided valuable information from which a therapy programme could be created. The Talking Mat also provided a visual representation of her perception of the issues before and after therapy, showing clearly her progress. This was well received by her parents, teachers and the other professionals involved in her care.
Once again I have been amazed by the power of the Talking Mat to produce a breadth of information in a relative short space of time and I will be advocating its use within cognitive assessment and rehabilitation across all ages.
Talking Mats is a useful tool to help parents see their child’s point of view.
The stage for each parent when their child also has an opinion about what is best for them can come as a surprise and is sometimes challenging. For parents of children with disabilities it can be even more so. This story is an example of how Talking Mats helped parents hear their own child’s voice amongst the background noise of the voices from health, education social and voluntary services.
David was in his final year of primary school. He attended a small village school and was transitioning to a large mainstream secondary. He has mobility problems due to cerebral palsy and uses a wheelchair. He can walk very short distances with effort using a walker and in his primary school used this method to move around the classroom and go to the hall for lunch and PE. This was a functional way to meet 2 of his targets : changing position and walking practise. His parents wanted this to continue when he transitioned to secondary school, although the health professionals involved felt it was going to be too difficult given the greater distances in the new building. An electric wheelchair was proposed for this new context. David’s parents were finding this next step challenging.
One of the professionals involved wanted to find out what David felt was important in his new school and used Talking Mats as a way of supporting him to think about various factors. The top scale used was ‘important/ not sure/ not important’.
David’s mat clearly showed that what was important to him in his new school was being with his friends. When his parents saw his mat they realised that this would be impossible if he was to move from class to class using his walker and it helped them make the transition to seeing him in an electric wheelchair. It also helped them see things from David’s point of view. They were more than happy to fit walking practise into a different part of his busy day because they had heard what was important to him.
Talking Mats allows different voices to be seen and heard.The name has been changed to protect identity.
Thanks to an OT colleague for this powerful story of how Talking Mats helped a woman with Multiple Sclerosis with goal setting by getting to the root of the problems she was having.
I am an OT working in a community rehabilitation team in Scotland. I have been seeing a woman (who I will call Jill) with MS. Jill has been experiencing increasing problems associated with her MS and finding it difficult to cope. During my first visit, Jill found it difficult to tell me about the problems she had been experiencing, and almost impossible to consider how we could translate these problems into tangible goals that we could work on. She was closed to any suggestions I made about potential rehabilitation goals. In her mind, the problems she had were there to stay, nothing could be done about them and she would just have to struggle on. We didn’t seem to be getting anywhere just talking about it. Jill was getting a bit exasperated and I was finding it difficult to keep a structure to our conversation and steer it towards agreeing on a goal that we could work towards. I felt there was a real risk of her disengaging from the service because we could not agree on a way forward.
Then I decided to use Talking Mats to see if that would help. I knew that using Talking Mats could help people with cognitive problems as well as those with communication difficulties. I wondered if doing a general Talking Mat using the Health and Well-being TOPIC symbols would help me identify what Jill thought her main problem areas were. Then I planned to do a sub-mat to look at her priority areas in more detail. My aim was to try and identify one or two rehabilitation goals (reflecting Jill’s priorities) that we could work towards. I really felt that there was potential to make a positive impact on Jill’s quality of life if I could get her to engage and agree on a goal to work towards.
Using Talking Mats proved to be a great success. Jill very quickly got the concept of it. It seemed to be much easier for her to pick up a symbol card, consider it, and then place it on the Mat. Using the Mat appeared to reduce the ‘cognitive load’ of the conversation and gave her structure to work within which she found much easier. Jill was able to identify what her main problem areas/ priorities were: – Mobility and Learning/ Thinking (see picture of her Mat above). Jill was pleased that she had got her message across and actually seemed to enjoy the process of using Talking Mats.
Now we have got a starting point. In my next session I’m hoping to complete sub-Mats with Jill in the Topics of Mobility and Learning/Thinking. This will allow us to explore these areas in more detail. Using Talking Mats was a real breakthrough in Jill’s rehabilitation.
To read another blog about using Talking Mats with someone with Multiple Sclerosis click here
We’re delighted that Andrea Powell, an Occupational therapist in Edinburgh has written a Blog for us about her experiences of being involved in group work with people who use AAC.
As a student occupational therapist, I worked part time as a support worker with an amazing lady Jennifer, (Jennifer is a pseudonym) Jennifer just happened to use an iPad to communicate. At this time I was about to commence my final year studies and was required to research and write a dissertation on a subject of interest. The lightning bolt of inspiration came when I, with Jennifer attended a weekly AAC user support group which was run and organised by a group of SLT’s.
The group was a wonderful resource that truly benefited the people who used it. I witnessed how much Jennifer valued spending time chatting with friends who also used an AAC device and who understood the unwritten rules of engagement. Such as patience while I set up my speech, don’t look at my screen while decide what I want to say etc. Her confidence in using different types of conversation grew while attending the group. It encouraged her to add to her already wide and variety vocabulary. As her support worker I also valued the opportunity to gain access to training on how to use her AAC and how I could provide better support to her.
I began reading around AAC and how people integrate of devices into their lives. I was however shocked to find that the wonderful group Jennifer attended was a rare occurrence for many users. The more I read, the more I realised that many users struggled to continue using an AAC device due to lack of support, access to trained professionals and most did not have wonderful resources like user support groups.
As an OT I was interested to explore the role in which I would play within AAC provision and found that as an OT I would be mainly providing support and advice on positioning, accessing devices and ergonomic type support.
However I felt that as an OT we have many more skills that didn’t appear to be to be getting utilised, within in my dissertation proposal I postulated that OT’s could expand their role within AAC to i) collaborating on assessments for AAC; ii) training on devices once they have been issued to users; and, iii) running and facilitating groups for AAC users and communications partners in the community.
OT’s are highly trained specialists skilled at understanding what is achievable and realistic for an individual. Occupational therapists assess individuals holistically in order to establish realistic and manageable goals which can be graded and adapted to suit the individual. Through the utilisation of appropriate grading of an occupation, a user can experience success and therefore less failure and frustration, ensuring the challenge is set at the appropriate level for the individual concerned (Park 2009).
Running and facilitating groups as a therapeutic tool is something that occupational therapists have been doing since the earliest days of the profession and groups are now utilised in many areas of practice (Howe and Schwartzberg 2001). By continuing this tradition, occupational therapists are well placed to take the lead in running and facilitating groups for AAC users, integrating social and community activities into the groups, for example, meeting in local shops to provide real life experience of interactions and, importantly, promoting the use of AAC to the general public. There are similar projects being attempted in Motherwell to increase the awareness of Dementia and make local businesses “Dementia friendly” (Shafii and Crockett 2013). Providing groups for AAC users not only enables them to learn how to use their devices, but also provides a support network of other users and communication partners.
I feel that if the skills of an OT were utilised in more than ergonomics then more positive outcomes could be seen for the user of AAC. I believe that if there were more OT’s taking on additional roles within AAC provision it could help reduce the pressure for SLT’s and the waiting lists to see SLT’s. It would also enable more users to be assessed to use AAC.
 Online training login
Online training login