Rachel Woolcomb, our Talking Mats OT Associate, tells us about the recent Royal College of Occupational Therapists’ Report and considers the ways Talking Mats can support:
The Royal College of Occupational Therapists have recently published a new report. “Making personalised care a reality: The role of occupational therapy.”
As the OT Associate for Talking Mats, I took the opportunity to review the document and consider how Talking Mats can help OT’s in fulfilling the recommendations made.
The report recognises that people living with long-term conditions bring different and equally important, knowledge and expertise to the decision –making process.
It challenges OT’s to ensure that they really listen to, and hear the views of the people they work with.
A Talking Mat can help facilitate this. It helps people to understand what is being discussed, to reflect and organise their thoughts, to say what matters most to them and record their views. It helps OT’s to really listen, to learn new information, to involve the person in their own planning and support decision making.
Read more about how Talking Mats can help OT’s to make personalised care a reality in the TMOT Resource 1: TM Personalised Care – Copy.
The RCOT report is available here: https://www.rcot.co.uk/news/delivering-personalised-care-frontline
Rachel would love to hear from you if you have any examples of how Talking Mats have helped you to provide personalised care, or if you want to know more about OT and Talking Mats. Her email is: Rachel@talkingmats.com.
If you are feeling inspired and would like to find out about accessing Talking Mats Foundation Training, take a look at our upcoming courses across the UK, as well as online and organisational training options: https://www.talkingmats.com/training/
Many thanks to Mary Walsh, Health Service Executive (HSE) Senior SLT at St Mary’s Hospital, Dublin for this fantastic blog post about their project involving use of Talking Mats to support people with Dementia to participate in decision making related to their needs:
In September 2016 Aideen Lawlor (SLT Manager) and I (Senior SLT) won the Dementia Elevator award with a project entitled “Empowering Persons with Dementia to become more Active Participants in Decision Making Related to Their Present and Future Needs.” with Talking Mats being an integral part of this project. In November 2017, the prize money was used to fund my training to become an accredited Talking Mats trainer so that I could then train others in TM Foundation Course on a prioritised basis.
This project is now complete with 6 speech and language therapists (SLTs) from a variety of settings working with persons with dementia all trained in using Talking Mats. As part of their training, The SLTs used TM with patients/ residents with particular reference to the Assisted Decision Making (Capacity) Act 2015. TMs were also used to help the clinicians to get to know their patients, in care planning, in improving increased opportunities for interaction and in improving choices and decision making. In effect, we were checking it out!
All the SLTs found that when TM principles are followed, that it helped to empower people with dementia to make decisions about their care. Some of the reported findings:
- That the pictures help maintain attention and aid comprehension.
- That it facilitated strengths rather than a deficit model.
- That photographed completed TM provided a pictorial record for meetings – very positive.
- That it provided a significant catalyst for change in some instances.
- That it helped people with dementia and responsive behaviour get needs met
- That video recording sessions with consent greatly enhances reflective practice and may be helpful in key decision making
The next phase is to expand the number of SLTs who can provide training in Talking Mats across the Republic of Ireland. Funding from the national SLT professional body training grant scheme has been sought for these 6 SLTs to become trainers for Talking Mats. This will result in cascading training on a priority basis, increase evidence base/ knowledge re using TM and embedding TM in variety of clinical settings with SLTs leading this practice.
Mary Walsh,
Senior speech and language therapist,
St. Mary’s Hospital,
Phoenix Park, Dublin 20,
Ireland
Aideen Lawlor
Speech and Language Therapy Manager
If you are feeling inspired and are interested in accessing Talking Mats training, we offer Foundation Training courses throughout the UK and Ireland as well as online – take a look here for more details:
Once you have accessed Foundation Training you can apply for our Accredited Trainers course to enable you to deliver Talking Mats training to others in your area.
We are delighted to introduce Rachel Woolcomb our first Talking Mats OT Associate. She is joining the Talking Mats Team and will be working to develop awareness and use of Talking Mats by Occupational Therapists. I will let Rachel introduce herself:
I am delighted that Talking Mats have asked me to join their team for one day a week. I am passionate about occupational therapy and about Talking Mats and to have the opportunity to bring these two loves together and seeing what develops is very exciting.
I live in South Gloucestershire and have had a varied career since I qualified as an Occupational Therapist in 1992. I was introduced to Talking Mats in 2008 and have never looked back, using them with my clients ever since.
In 2017, having spent over 25 years working in the NHS, I made the decision to move into independent practice. I work predominately with teenagers and adults who live with long term neurological conditions or who have experienced catastrophic injuries following trauma. I am very aware of the psychological impact of sudden disability and the need for people to be able to express who they are and what is important to them, even in difficult circumstances.
I now use Talking Mats with most of my clients. It doesn’t matter if they are old or young, can speak or have communication needs, they all benefit from the opportunity to stop and think and have someone really listen to them.
In the last few weeks a man who has had a stroke and has limited expressive speech has used a Talking Mat to talk about what leisure activities he used to enjoy. He then used a second mat to explain what he can and cannot achieve now. This helped us together, set goals for occupational therapy. I am also working with a teenager who has had a traumatic brain injury and now struggles with her education. She uses Talking Mats with me regularly, to think about her coping skills at school. Looking back at her previous mats is helping her to recognise progress. I have so many more examples and will be sharing them with you soon!
I really want to inspire OT’s, helping them to consider how they enable their clients to think, communicate their choices and make decisions. A Talking Mat is a great for this. It is also creative and interactive something that in my experience OT’s like! I will also be looking at important issues within the field of occupational therapy that are currently driving practice, such as personalised care, goal setting and shared decision making. I believe it is vitally important that we collaborate with our clients as together we can achieve so much more. Talking Mats is an effective tool in enabling this, so watch this space, and please do get in touch if you want to know more or have stories to share.
It is great to have Rachel working with us to build on some of the excellent work being done already in the Occupational Therapy Sector. Our Director, Lois Cameron shares why we are so excited to welcome Rachel to our Team:
‘I am really pleased that Rachel is joining us . I think the Talking Mats approach sits well with the values and approach of Occupational therapy, In my experience OTs are naturally holistic in their approach. I remember at a training course in London an OT said for her Talking Mats was the missing link in her toolkit. The training and experience of OTs allow them to see things through a different lens and that will be really helpful to us’
For more information about how OT and Talking Mats are a winning combination, take a look at Rachel’s recent blog – https://www.talkingmats.com/talking-mats-and-ot-a-winning-combination/
Feeling inspired and want to know more about the training courses we offer? See www.talkingmats.com/training/ for details.
In Stockport we have a termly ‘Voice of the Child/Young Person’ Champions Network meeting during which professionals working in health, education and social care settings across the area meet to discuss real-life examples and to share information and strategies – during the last meeting in October 2018, we discussed using Talking Mats to support police interviewing.
Louise Tickle, Specialist Learning Disability Nurse from the Children’s Learning Disability Team at Stockport NHS Foundation Trust, shared a great example of using Talking Mats to support a child she was working with to share information about a serious safeguarding concern. Louise had been asked by the police to carry out a Talking Mats session with the child as they were aware that she was already using this approach. Louise led the session and was supported by the child’s school SENCO, who had also been Talking Mats trained. The aim was to explore a disclosure which the child had previously made.
Louise shared some great tips about using Talking Mats during an investigation phase:
- Introduce the Talking Mat with a familiar topic, then move on to the main topic/ area of concern
- Watch out for non-verbal cues – initially, the child appeared to be happy and relaxed during the interview, however the child’s non-verbal communication visibly changed when the topic changed. It is easier to pick up on these non-verbal cues if you are able to video the session.
- Have another Talking Mats trained observer present if possible to support and evaluate the session with you.
- Make sure you use terminology that the child is familiar with, and use language that the child would use themselves e.g. when describing body parts.
Talking Mats are often used by people working within the justice system, including registered intermediaries – here is the link to one of our previous blog posts for more information: https://www.talkingmats.com/talking-mats-used-court/.
In this work you must be clear about the different stages of safeguarding and follow the procedures within your organisation. Disclosure and investigation are two different phases. The Keeping Safe resource has been trialled and tested to support people to raise concerns. https://www.talkingmats.com/keeping-safe-a-new-talking-mats-resource-available-to-purchase/ . When a disclosure moves to the investigation phase you may have to personalize the mat to fit the situation but what is key is that you keep the options open and non-leading.
For further information about accessing one of our Talking Mats Foundation Training Courses across the UK, and our ‘Keeping Safe’ Advanced course, see our training options here https://www.talkingmats.com/training/
Find out about the Core and Essential Service Standards for Supporting People with Profound and Multiple Learning Disabilities. and thanks to Joanna Grace for this interesting and important guest blog ,she writes;
Last week I threw used deodorant canisters at an audience of earnest professionals and was cheered for doing so. What was going on?
I run The Sensory Projects an organisation that aims to share the knowledge and creativity required to turn inexpensive items into effective sensory tools for inclusion. In all I do I am working to contribute to a future where people are understood in spite of their differences.
The empty deodorant canisters had been washed, their roller balls removed to enable me to fill them with festive scented balm – some frankincense some myrrh – with balls replaced they make wonderful massage tools enabling me to form a connection through touch and smell with persons of all abilities and to share a sensory conversation around the season.
I lobbed them at my audience to bring to life the new Core and Essential Service Standards for Supporting People with Profound and Multiple Learning Disabilities. That title might not sound exciting and the link with my improvised massage tools might not be immediately apparent but I promise you the link is there and the document is very exciting indeed.
My original dream when I set up The Sensory Projects was to write five sensory stories. That dream was a bit of a fantasy and so I had to pinch myself when it came true. The original five stories are sold to fund the writing of more and there are now twenty available on the website. The stories led to books, of which there are five in print currently and a few more in the pipeline. The stories project led to another project, which led to another, and there are four currently and a fifth due to start next year. Through the projects I have had the chance to do some remarkable things and found myself in situations I never imagined I would be in: I’ve been featured in a book given away in Lush stores globally, I’ve been interviewed on Radio 4, I’ve done a TEDx talk, I’ve even exchanged text messages with the Foo Fighters! If I continued to pinch myself when remarkable things in my life happened I would be black and blue by now.
And yet of all of these wonderful things and the many adventures I have had, by far and away the best thing I have been a part of is the new Core and Essential Service Standards for Supporting People with Profound and Multiple Learning Disabilities.
The new Core and Essential Service Standards for Supporting People with Profound and Multiple Learning Disabilities is a document that describes what best practice care looks like when supporting people with profound and multiple learning disabilities. It is beautifully simply having just 7 standards for what best practice looks like at an organisational level and 6 standards for what it looks like at an individual level. It was written by a team of volunteers over 140 strong over an 18 month period. It represents an enormous work of effort and hope. I am humbled and proud in equal measure to be one of its four lead authors. If adopted by the inspecting agencies it would change the face of what care looks like for individuals with complex disabilities nationwide and influence care provision globally.
Even without being adopted by the inspecting bodies it is having an impact. I encourage all settings to take a look at it. If you are a great setting celebrate that you meet the standards, declare it publicly, display it on your website, tell the world – and help us to create an expectation that this is what care should look like. If you are a middling setting celebrate that you are working towards the standards, use them as a reflective tool to drive up the quality of care that you offer. And if you work in a duff setting….well, I spoke to one woman who worked in a setting where the management were thoroughly uninterested in supporting their residents with profound and multiple learning disabilities. She looked through the document, thumbing the forward by Norman Lamb and the endorsement by NHS England, she gave me a wry smile “I don’t think my boss will know this isn’t legal” she winked, “I’m just going to give it to him!” However the change comes about, we want to see these standards upheld.
Early on in the writing process we had to make a decision: were we going to describe what best practice care looked like now, or what it ought to look like. We went with what it ought to look like. This is an aspirational document. But that is not to say it is unachievable. I cannot emphasise the “ought to” strongly enough. The first standard for individuals is communication, within the explanation for this standard is the following: “Communication should be a collaborative activity, it has to be a two-way exchange; reciprocal and responsive.” That is not asking a lot. It is a shame on our society that such basic standards are aspirational at all. It should already be happening.
We launched the standards at an event called Raising the Bar last year. Raising the Bar II was held this year and looked at how far we had come since the launch. One speaker told the room full of delegates “before you seek to raise the bar you must allow family members to say where the bar is currently” and we did. Families presented about the level of care their loved ones had received and their stories were horrific to hear. The bar is currently set very very low. Standards such as two way communication are aspirational. It is so low that it should be easy to raise. Simply by being aware of what we should be doing, making others aware, and expecting to see positive change we can go some way to improving care. Raising the Bar III is due to be held at Birmingham University next year on the 25th of October.
Most importantly of all we want families and primary carers to know about the standards so that they can use them as an advocacy tool and demand that settings meet them. There is a community of practice hosted on Facebook that networks people working together to see this change come about. Please join us.
So what was the deodorant canisters thing about? Well a two way communication for someone who does not use words can begin at a sensory level. It can be me massaging your hand with a festive scent and watching for your response. To be truly two way I need to share this time with you on multiple occasions as your responses today might be indicative of something other than your opinion of this scent. They could be a pain in your stomach, a tightening of a muscle, a epileptic shudder. To truly know your response, your opinion, to truly make the communication two way I need to repeat, and to give you time, and to tune in to your response and then I need to listen to it and act upon it. If through our conversations you tell me you like one smell and dislike another then this will help me choose from the pile of toiletries you are given for Christmas which you will really enjoy. As I share these simple conversations with you over time I address another of the standards:
Standard two is about health and wellbeing and describes how staff will have an awareness of what good mental health looks like for an individual and how to support it. Smell has a particularly powerful effect on the emotions and fostering an engagement with smell is a good way of supporting someone’s mental health – regardless of their ability, disability or neurodiversity. On my Sensory Engagement for Mental Well Being training day I look at many simple sensory strategies for supporting mental health for people with complex disabilities.
A document like the standards can seem dry and impersonal, throwing things at my audience helped me to bring it to life. My whole working life, and much of my private life – I have worked for inclusion in mainstream education settings, I have taught in a school for children with severe and profound special educational needs and disabilities, I have inspected schools for their provision for children with additional needs and provided consultancy services to schools looking to improve their provision, I have family members with neurodiverse conditions and physical disabilities, I have been a registered foster carer for children with severe and profound special educational needs and disabilities and I have run The Sensory Projects – has been about working to see people be better understood, better included and better appreciated for being themselves. The Standards are the pinnacle of all of this work.
You can download the Standards for free from the PMLD link website: www.PMLDlink.org.uk by following the ‘Resources’ tab, or from my own website www.TheSensoryProjects.co.uk – again follow the Resources tab. Please print them off and share them far and wide, make sure everyone you know who is involved in the lives of people with profound and multiple learning disabilities, or has influence over their lives in anyway, knows about them. Together we will create this change.
I also warmly invite you to join us on the Community of Practice, let us know who you have shared the Standards with, it is great to hear what others are doing.
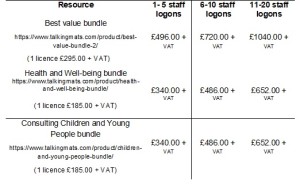
The Talking Mats digital app is available for organisations to purchase. This is an efficient way to support staff to evidence person centred planning.
The digital app typically operates via individual logons which means personal data is kept securely and it complies with data protection and client confidentiality. The individual with the logon can use their Digital Talking Mat with as many client/patients as they want.
We recognise that organisations may want to purchase several logons for staff to access digital Talking Mats and for that reason have created an Organisational Talking Mats digital licence. The savings are significant.
For application criteria please contact the Talking Mats office on 01786 479511
We are grateful to Rachel Woolcomb OT, for sharing this Talking mats story.
Within my occupational therapy practice I have found Talking Mats to be an excellent thinking tool to help my clients establish their priorities for therapy.
I was asked to work with a teenage girl who had sustained a brain injury resulting in a mild cognitive impairment which was impacting on her participation and ability to learn at school.
She had undergone formal cognitive testing with a clinical psychologist, however had shown poor levels of engagement with the assessment process (which had taken over two hours). She was reported as having erratic focus and inconsistent answers to questioning. The results were therefore deemed to be inconclusive and no recommendations made. I knew that Talking Mats would provide me with similar information to that which the psychologist was trying to gain, but in a way that would be engaging and client focused. I also felt that the concept of the Talking Mat, which enables the thinker to express their own views rather than a “right or wrong” answer, would help to improve participation.
I selected the learning and thinking topic cards from the communication set within the Health and Wellbeing pack. These cards cover areas that I would normally look at within any cognitive assessment and are functionally relevant. Together we selected the visual scale, choosing the question “how well are you managing?”
She explained that organising herself, writing, listening, reading, problem solving and planning were all going well. She talked about how she sometimes had difficulties concentrating and paying attention due to getting distracted in the classroom. She also felt she was struggling more than before with calculating and that this was affecting her scores in Math tests. She explained that remembering and making decisions were “not going well’ and she was particularly worried about the fact she had forgotten some of the teaching she had received prior to her brain injury. I was also able to conclude from the way she understood the concept of the mat, as well as her ability to engage and attend for the whole session, that she could concentrate, learn new skills and had the ability to weigh up information to help her make decisions.
Together we used the information gained from the Talking Mat to set goals for therapy which were focused around having a range of strategies to help her concentrate in class, remember new information, and make decisions.
Two months later, once having completed a therapy programme, we used the Talking Mat again to explore her current thinking about the topic area. She explained that making decisions was something she no longer had difficulty with as her confidence had grown. She felt that there had been some improvement with her ability to remember information and we discussed the strategies she now used to help her concentrate in class, which included ways to minimise any distractions.
In summary, the Talking Mat enabled her to think about how her brain injury had affected her ability to remember, make decisions and learn. This provided valuable information from which a therapy programme could be created. The Talking Mat also provided a visual representation of her perception of the issues before and after therapy, showing clearly her progress. This was well received by her parents, teachers and the other professionals involved in her care.
Once again I have been amazed by the power of the Talking Mat to produce a breadth of information in a relative short space of time and I will be advocating its use within cognitive assessment and rehabilitation across all ages.
Our next train the trainer course is in 2 weeks and we’re looking forward to welcoming people from a range of professions and a range of places- New Zealand, Japan, England and Fife!
Becoming a trainer for Talking Mats means the staff member can offer Foundation training within their organisation or partnership. This ensures that the standard of the communication and thinking tool is maintained and sustainability of its use is supported. It is a positive investment for organisations in person -centred practise.
The trainers are provided with resources for delivering the Foundation course and their licence is renewed annually .
Comments from people who attend include:
Practical approach to training made it easy to try out and learn from ‘doing’
A wonderful inspiring course- really looking forward to continuing to work as part of the TM team
Really enjoyed the training. Learnt a lot not just about my use of TM but also just about myself as a presenter and communication
If you’ve attended a Foundation course and would like to become a trainer, our next course is in June. You can find out more details on our webiste or on this link 20180621 Accredited Training flier Jun 2018
Thanks to Rosie Murray for this great blog describing how she used a collaborative Talking Mats ‘Wall’ to help students comment on how different activities inside and outside college make them feel.
As a student, I trained in the Talking Mats approach, after finding it incredibly useful in clinical placements. I am now a speech and language therapist at St John’s College in Brighton. This is a college for young adults with autism, learning disabilities and SEBD. Our learners have a wide range of communicative needs and cognitive abilities. I was approached by our nursing team in the lead up to world mental health awareness day, as they were organising a ‘tea and talk’ session for our learners of all abilities.
We organised a range of activities, such as symbolised conversation starters. However, we felt we needed something to allow our less verbal learners to make their voices heard. I thought back to my training, and remembered Joan Murphy talking about large, collaborative Talking Mats – or ‘talking walls’. We discussed this idea, and felt it would be a great way for students to feedback on how different activities inside and outside college make them feel.
It took some considerable planning. Due to the emotional needs of some students, our top scale required us to avoid words that were too upsetting for individuals. In the end we settled on ‘good’ (with a widget ‘calm’ symbol) and ‘worried’. We also wanted it to provide a genuine opinion, so although we considered including activity options that were clearly negative, e.g. ‘fire alarms’, we took the opportunity to show our learners that we all have different opinions on things, and that this is good. We hypothesised that because of this, learners would be skewed towards giving positive opinions, and this informed the order of presentation of the top scale and the activities themselves.
On the day, we had 15 different activities to give an opinion on, each with different border colours for differentiation, and of course blank tiles so our learner’s could come with their own activities. Students were encouraged to write their name on the back of a chosen activity, and a consistent script was used to present the wall to each learner. Makaton signing was used alongside the script to support understanding.Learners of all abilities offered their opinion, and it generated discussion between learners of differing abilities. It signposted staff to particular likes and dislikes of learners, and showcased the power of talking mats to all staff. For example, one of our learners is a cheerful young man, who uses minimal verbal utterances to communicate. When the board was presented to him, he very clearly selected ‘talking’ as an activity, and clearly indicated that it makes him worried. This has allowed us to reflect as a staff team about how we can support him to communicate with minimal anxiety.
Learners too took away some important lessons from using the wall. They saw that while some activities are VERY popular (e.g. computer time), some are quite polarised, e.g. animals. This highlights the important issue of mutually respecting each others differences. Since the event, staff have discussed ideas they have on how to utilise this tool. We are considering how we could use Talking Mats as a tool in our peer mentoring sessions between learners of higher and lower verbal ability, as we feel it would be beneficial for both mentee and mentor. We are looking forward to using Talking Mats as a flexible tool for the college in the future.
Please let us know of any other innovative ways of using Talking Mats!
Talking Mats is a useful tool to help parents see their child’s point of view.
The stage for each parent when their child also has an opinion about what is best for them can come as a surprise and is sometimes challenging. For parents of children with disabilities it can be even more so. This story is an example of how Talking Mats helped parents hear their own child’s voice amongst the background noise of the voices from health, education social and voluntary services.
David was in his final year of primary school. He attended a small village school and was transitioning to a large mainstream secondary. He has mobility problems due to cerebral palsy and uses a wheelchair. He can walk very short distances with effort using a walker and in his primary school used this method to move around the classroom and go to the hall for lunch and PE. This was a functional way to meet 2 of his targets : changing position and walking practise. His parents wanted this to continue when he transitioned to secondary school, although the health professionals involved felt it was going to be too difficult given the greater distances in the new building. An electric wheelchair was proposed for this new context. David’s parents were finding this next step challenging.
One of the professionals involved wanted to find out what David felt was important in his new school and used Talking Mats as a way of supporting him to think about various factors. The top scale used was ‘important/ not sure/ not important’.
David’s mat clearly showed that what was important to him in his new school was being with his friends. When his parents saw his mat they realised that this would be impossible if he was to move from class to class using his walker and it helped them make the transition to seeing him in an electric wheelchair. It also helped them see things from David’s point of view. They were more than happy to fit walking practise into a different part of his busy day because they had heard what was important to him.
Talking Mats allows different voices to be seen and heard.The name has been changed to protect identity.
 Online training login
Online training login