In this latest blog, our Talking Mats OT Associate, Rachel Woolcomb tells us how Talking Mats can support delivery of Personalised Care:
“Person centred practice”, and “partnership approach” are common phrases heard in health and social care settings but what does this really mean in practice?
How good are we at ensuring our service users are truly heard, and given opportunities to talk about what is important to them?
Recently NHS England set out their ambitions for the delivery of personalised care. This is a commitment to enabling people to have the same choice and control over their mental and physical health that they have come to expect in every other part of their life.
This however requires a shift in culture.
One of the cornerstones of personalised care is shared decision making. This is a collaborative process in which people are supported to understand the options available to them including the various risks, benefits and consequences. A shared decision will have acknowledged personal preferences, circumstances, values and beliefs. This ensures that when a choice is made it is fully informed.
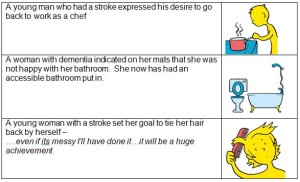
There is substantial literature which demonstrates the usefulness of goal setting as part of the communication and decision making process.
A well written person-centred goal will describe the anticipated achievement of a specific activity. It will be meaningful and help create a common vision within the rehabilitation process.
Talking Mats is an ideal tool to help facilitate these processes. They enable better conversations and provide an interactive thinking space. They have also been demonstrated to be a useful tool in enabling people to think about their rehabilitation goals.
Read more about this in the TMOT Resource 2: How Talking Mats can help facilitate shared decision making and goal setting: Goal setting TMOT 2
If you would like to find out more about the different Talking Mats training options we offer, take a look here: https://www.talkingmats.com/training/
Rachel Woolcomb, our Talking Mats OT Associate, tells us about the recent Royal College of Occupational Therapists’ Report and considers the ways Talking Mats can support:
The Royal College of Occupational Therapists have recently published a new report. “Making personalised care a reality: The role of occupational therapy.”
As the OT Associate for Talking Mats, I took the opportunity to review the document and consider how Talking Mats can help OT’s in fulfilling the recommendations made.
The report recognises that people living with long-term conditions bring different and equally important, knowledge and expertise to the decision –making process.
It challenges OT’s to ensure that they really listen to, and hear the views of the people they work with.
A Talking Mat can help facilitate this. It helps people to understand what is being discussed, to reflect and organise their thoughts, to say what matters most to them and record their views. It helps OT’s to really listen, to learn new information, to involve the person in their own planning and support decision making.
Read more about how Talking Mats can help OT’s to make personalised care a reality in the TMOT Resource 1: TM Personalised Care – Copy.
The RCOT report is available here: https://www.rcot.co.uk/news/delivering-personalised-care-frontline
Rachel would love to hear from you if you have any examples of how Talking Mats have helped you to provide personalised care, or if you want to know more about OT and Talking Mats. Her email is: Rachel@talkingmats.com.
If you are feeling inspired and would like to find out about accessing Talking Mats Foundation Training, take a look at our upcoming courses across the UK, as well as online and organisational training options: https://www.talkingmats.com/training/
This blog is about how Care Inspectors in Sweden are using Talking Mats.
On 18th March I met up with old friends – Ulrika Ferm and Eva Holmqvist – at the ISAAC Denmark Conference in the beautiful Vingsted Conference Centre in West Denmark. Ulrika and Eva work at DART Communication Centre in Gothenburg Sweden http://www.dart-gbg.org/english/.
I was giving a presentation on new developments in Talking Mats and as always happens when we meet, we talked non stop about families and work.
Ulrika told me about the following initiative in Sweden and we agreed it would be useful to write a blog about it.
The Health and Social Care Inspectorate https://www.ivo.se/ (the Swedish equivalent of the Care Commission) had been in touch with DART about how they could get the views of people with dementia who live in care homes.
DART made a program of communication for the inspectors which included a first day about communication and dementia. Following this there was a full 2 day course on Talking Mats for 15 inspectors who then went on to pilot the use of Talking Mats as a way to get the genuine views of residents. It was so successful that they are planning to roll this out elsewhere. Now more inspectors in Sweden are getting Talking Mats training and using pictorial support as preparations before inspections.
It would be really good if this could happen in Scotland.
Many thanks to Mary Walsh, Health Service Executive (HSE) Senior SLT at St Mary’s Hospital, Dublin for this fantastic blog post about their project involving use of Talking Mats to support people with Dementia to participate in decision making related to their needs:
In September 2016 Aideen Lawlor (SLT Manager) and I (Senior SLT) won the Dementia Elevator award with a project entitled “Empowering Persons with Dementia to become more Active Participants in Decision Making Related to Their Present and Future Needs.” with Talking Mats being an integral part of this project. In November 2017, the prize money was used to fund my training to become an accredited Talking Mats trainer so that I could then train others in TM Foundation Course on a prioritised basis.
This project is now complete with 6 speech and language therapists (SLTs) from a variety of settings working with persons with dementia all trained in using Talking Mats. As part of their training, The SLTs used TM with patients/ residents with particular reference to the Assisted Decision Making (Capacity) Act 2015. TMs were also used to help the clinicians to get to know their patients, in care planning, in improving increased opportunities for interaction and in improving choices and decision making. In effect, we were checking it out!
All the SLTs found that when TM principles are followed, that it helped to empower people with dementia to make decisions about their care. Some of the reported findings:
- That the pictures help maintain attention and aid comprehension.
- That it facilitated strengths rather than a deficit model.
- That photographed completed TM provided a pictorial record for meetings – very positive.
- That it provided a significant catalyst for change in some instances.
- That it helped people with dementia and responsive behaviour get needs met
- That video recording sessions with consent greatly enhances reflective practice and may be helpful in key decision making
The next phase is to expand the number of SLTs who can provide training in Talking Mats across the Republic of Ireland. Funding from the national SLT professional body training grant scheme has been sought for these 6 SLTs to become trainers for Talking Mats. This will result in cascading training on a priority basis, increase evidence base/ knowledge re using TM and embedding TM in variety of clinical settings with SLTs leading this practice.
Mary Walsh,
Senior speech and language therapist,
St. Mary’s Hospital,
Phoenix Park, Dublin 20,
Ireland
Aideen Lawlor
Speech and Language Therapy Manager
If you are feeling inspired and are interested in accessing Talking Mats training, we offer Foundation Training courses throughout the UK and Ireland as well as online – take a look here for more details:
Once you have accessed Foundation Training you can apply for our Accredited Trainers course to enable you to deliver Talking Mats training to others in your area.
Talking Mats received funding from The Health and Social Care Alliance Scotland to look at how using the Digital Talking Mats can help people with long term conditions, including dementia, to manage their health and well-being and to recognise their own strengths and abilities. We also hoped that participants would be able to have more control over their lives and have improved communication with families and professionals.
11 people living with dementia and their partners were involved in the project. Each participant had a tablet device and was given a personal digital Talking Mats licence which gave them access to 13 topics in the Talking Mats Health and Well-being resource. We visited each participant at home, taught them how to use it and asked them to complete at least 1 digital Talking Mat per week for 6 weeks on any topic they wished. The design of the digital Talking Mat allowed them to email their mats directly to us. We visited each participant a second time to discuss how easy it was to use the digital Talking Mats and their views on their completed mats. We asked those who wished to, to continue sending us completed mats beyond the initial 6 weeks and we visited them again in 6 months to discuss how they were managing.
In total we received 94 digital mats across all 13 topics from the participants living with dementia who reported that the use of the Digital Talking Mats during this project gave them a better understanding of their own individual health and social care needs.
A woman with dementia said ‘It (Health mat ) made me realise things are not so bad and made me think I will continue with my exercise classes, carry on walking, socialising and eating well’
As well as helping participants self-manage their lives, an unexpected outcome of this project was that many people found that using the Digital Talking Mats helped them see the positive things in their life and not just the negative. It also highlighted that despite having a deteriorating illness, things were not getting worse.
‘This mat (Environment) showed me how happy I am in my own home and my neighbourhood’
The following are some of the comments we received throughout the project.
• It helps me sort out my thoughts – very useful
• I get so much out of the process
• I come up with insights which might help me in the future
• I can now talk to (my wife) in a way I couldn’t before
• I’m more relaxed now
• I come up with niggly health things that my partner didn’t know
‘It made me realise things are not so bad’.
If you know of anyone living with dementia would like to obtain the Digital Talking Mats please fill in the attached Personal Digital Licence 161117 DTM personal licence form with explanation and send it to us at info@talkingmats.com
Self-management for people with long term conditions (LTC) is now a key government strategy to encourage people to take responsibility for their own health, behaviour and well-being. Talking Mats received funding from The Health and Social Care Alliance Scotland to look how using the Digital Talking Mats (DTM) can help people with LTCs to manage their health and well-being and to recognise their own strengths and abilities.
The overall aim of our project was to empower people with different long term conditions, to manage their own health and well-being. Through using Digital Talking Mats (DTM) we hoped that participants would be able to have more control over their lives and have improved communication with families and professionals.
There were a total of 28 participants in this project living with one of three different long term health conditions – stroke, dementia and learning disability. Each participant had access to a tablet device and was given a personal DTM licence which gave them access to 13 topics in the Talking Mats Health and Well-being resource. We visited each participant at home and taught them how to use it and asked them to complete and send us at least 1 digital mat per week for 6 weeks on any topic they wished. The design of the digital Talking Mat allowed them to email their mats directly to the researchers. We visited each participant a second time to discuss on how easy it was to use the digital Talking Mats and their views on their completed mats. We asked those who wished to, to continue sending us completed mats beyond the initial 6 weeks. We visited them again in 6 months to discuss how they were managing.
15 participants completed all 6 mats and 12 participants continued to complete mats over the length of the project. Participants completed 235 digital mats across all 13 topics
There were 3 particularly significant findings
1. At 18 months the participants living with dementia actually felt their well-being had improved, despite dementia being a progressive illness.
2. For the participants living with stroke the results were even more striking as 95% felt things were going well at the end of the project in comparison with 47% at the beginning.
3. At the end of the project the percentage of people with learning disability who felt things were not going well had reduced from 19% to 10%. Furthermore the percentage of people indicating that they were not sure about their views had increased from 27% to 42%. There can be a tendency for people with learning disability when using Talking Mats, to express their views at either end of the mat and to rarely use the mid- point. However being able to use the unsure mid- point is noteworthy as it indicates that the participants in the project realised that they could express their views not only as black or white but could indicate that they were unsure. This awareness opens up the potential for people to express views more thoughtfully with opportunities for further exploration.
Here are three examples of how using the DTM supported people to self-manage situations in their lives. Click on image to enlarge.
As well as helping participants self-manage their long term conditions, an unexpected outcome of this project is that many people found that using the DTM helped them see the positive things in their life and not just the negative. It also highlighted that despite having a long term condition and, for many also a deteriorating one, that things were not getting worse.
Click here for full report including 6,12 and 18 month reports to the funders 20180717 Alliance full report
Click here for the summary report 20180717 Alliance Final Short Report
Click here for a video link of 2 participants
Many thanks to Elaine Hunter, National Allied Health Professions Consultant with Alzheimer Scotland for this blog
Background
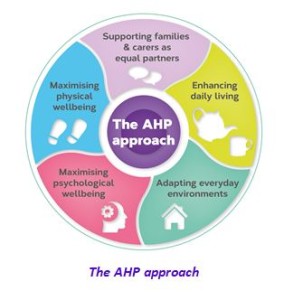
Connecting People, Connecting Support is a new policy document in Scotland and shares how allied health professionals (AHPs) in Scotland can support people with dementia, their families and carers to live positive, fulfilling and independent lives for as long as possible.
The policy document presents an evidence-informed case to support a biopsychosocial approach to practice for ALL AHPs in Scotland when working with people living with dementia – what we call the AHP approach. The fundamental understanding driving the AHP approach is that people living with dementia CAN benefit from AHP-led interventions. In this week’s blog we are sharing the AHP contribution to maximising psychological wellbeing.
Maximising Psychological Wellbeing
What do we mean by psychological wellbeing?
The central importance of finding ways to communicate (verbal and non-verbal) that work for each individual and which make meaningful connections that may have wide-ranging benefits in relation to overall wellbeing and quality of life is recognised. Psychological interventions of different intensities are reflected to promote emotional health and psychological wellbeing, with the provision of psychological interventions for depression, anxiety, and expressions of stress and distress. This element builds on established AHP psychological interventions and therapies.
Why is psychological wellbeing important?
People with most types of dementia will at times struggle to find the right words or follow a conversation.
- Communication difficulty can be exhausting for the person, families and carers
- We know that people can often find it difficult to talk about dementia and many people living with dementia experience social isolation
- Dementia can have a profound psychological impact and may be linked to feelings of anxiety and depression.
- A non-pharmacological therapeutic approach is advocated for the treatment of psychological symptoms and a person-centred stepped-care model of support.
3 ways allied health professionals CAN maximise psychological wellbeing?
1. Maintain and maximise communication
AHPs are aware that optimum communication occurs in environments that are comfortable, where a person can feel relaxed and safe, and when the AHP-led intervention is tailored and individualised. AHPs have experience in training others in conversation skills and cuing strategies, identifying key elements for effective everyday communication and supporting opportunities to practice communication strategies in a social context, helping the person to gain confidence in the interaction. Speech and language therapists can provide personalised communication advice (aimed at, for example, developing communication passports, assessing communication networks and maximising communication opportunities) that is shared with family members to facilitate their communication skills. Where language difficulties present as a primary feature of the dementia, as in primary progressive aphasia, speech and language therapists will carry out assessments to identify specific communication impairments and abilities. Their findings will contribute to the diagnosis and be used to plan therapy and strategies.
2. Psychological interventions
AHP core psychological skills are unique to each profession and vary according to their undergraduate education and postgraduate development activity. AHP interventions to maximise psychological wellbeing require excellent communication skills and the ability to integrate psychological interventions and psychological therapies into core AHP practice. A number of approaches based on the psychological understanding of dementia and its effects, including reminiscence approaches, life-story work, anxiety management, and engaging in everyday occupations and activities, will be core to AHPs’ day-to-day practice.
With additional enhanced training opportunities, psychological interventions can also become core to AHP roles and integral to a team approach to a stepped-care model of assessment and intervention. Psychological interventions include motivational interviewing, behavioural activation, mindfulness based cognitive therapy, cognitive stimulation therapy, cognitive rehabilitation and cognitive behavioural therapy. Specific psychological interventions providing individualised, formulation-led interventions in response to stress and distress in dementia, ranging from low-intensity to specialist interventions, can also be within AHP remits.
3.Psychological therapies
Psychological therapies are highly specialised psychological interventions that include the established AHP disciplines of art psychotherapy and music therapy.
Art psychotherapy creates opportunities for verbal and non-verbal communication by using art to enable people to feel connected to a sense of self, other people and the environment around them. It can support people living with dementia by reducing anxiety and increasing coping skills (Safer & Press, 2011), depending on how interested the person is in art activities, art materials and how they feel about one-to-one or group activities. Art psychotherapy can be particularly helpful for people who find it hard to express their thoughts and feelings verbally, enabling self-expression and enhancing sense of self and personhood.
Music therapy builds on people’s ability to respond to music to develop a therapeutic relationship and facilitate positive changes in emotional wellbeing and communication through engagement in live musical interactions. It has a robust evidence base as an effective, non-pharmacological intervention that can significantly improve and support the mood, alertness and engagement of people with dementia, reduce the use of medication, and help to manage and reduce agitation, isolation, depression and anxiety (Ridder et al., 2013).
These art-based therapies are particularly helpful when people find their emotions are too confusing to express verbally, when verbal communication is difficult or when words are not enough.
Supervision for the AHP professions is integral to all of the interventions.
On reflection
Thank you for taking the time to read this blog and we would like to know
- As an AHP, how do you currently support people living with dementia to maximise the persons psychological wellbeing?
- As person living with dementia, what support would you like to receive from allied health professionals to maximise your psychological wellbeing?
- As family carer, what support would you like to receive from allied health professionals to maximise your psychological wellbeing?
We look forward to hearing from you.
Email me at EHunter@Alzscot.org
References
There are references supporting this text which you will find in the original policy document and can be viewed here https://www.alzscot.org/assets/0002/7356/AHP_Report_2017_WEB.pdf with all the evidence informing the policy available at www.alzscot.org/ahp
Talking Mats were delighted to be involved in the launch of Care Opinion’s Picture Supported stories at the Life Changes Trust Gathering in Perth Scotland this week. We have been working with Care Opinion for the past two years to develop this feature. This earlier Talking Mats blog describes the development process and this recent Care Opinion blog gives some examples of the feature in use.
However, in this blog, I want to reflect on two events I went to within a short space of time; the gathering in Perth on Monday and the Royal College of Speech and Language Therapists study day the previous thursday in Stirling . It felt to me like my two worlds colliding or maybe it was just my stars aligning ! At the RCSLT study there was a session on the public perception of Speech and Language therapy and how there is still much work to do in changing the myths that are spun and repeated about what Speech and Language therapists actually do . For as John F Kennedy said in 1962 ‘ the great enemy of truth is very often not the lie but the myth , persistent, persuasive and unrealistic ´ The National Allied Health Professional children’s lead, Pauline Beirne suggested to the study day that Care Opinion is a great web site for encouraging that sharing of stories. Then, strangely when I got back into the office there was a story waiting for me in my in box all about the positive experience of a parent involved in a Hanen programme in NHS Lanarkshire which reinforced that very message.
We know people relate to stories, stories resonate and have impact, they are easy to remember . Our drive in working in partnership with Care opinion was to support more people to tell their health and care stories by increasing accessibility . It was designed with and for people with dementia through funding from Life Changes Trust but anyone can use it and they are! It is great to see the stories coming in.
Through stories let’s celebrate the good, develop and improve practice and let’s use stories to challenge myths and educate. So use Care Opinion and try out the picture supported stories to share your experiences , tell other people ,spread the word and the picture supported story feature !
We have been working with Care Opinion to develop the accessibility of their site for people with dementia through picture supported stories.We are very grateful to Life Changes Trust for funding this partnership.
What is Care opinion ?
Care Opinion is an independent third sector organisation that supports feedback on health and care services. They promote honest and meaningful conversations between users of health and care services and their provider organisations. If you want to see how Care Opinion works then take a moment to watch this excellent video
Why is our partnership important?
Both organisations believe it is important that everyone can tell the story of their experience of using health and care services. This can be hard as there can be barriers to telling a first-hand account of an experience. These barriers can include
- difficulties with expression and finding the correct words
- difficulties with memory
- difficulties with writing or typing on a computer
Care Opinion is skilled and experienced in supporting feedback through their web platform and supporting health and care improvements through responding to and sharing that information . Talking Mats is skilled and experienced at supporting people with communication difficulties including people with dementia, to express their views. Partnership working between the two organisations has enabled a fusion of ideas and learning from each other to develop and action our vision of a care opinion platform that is more accessible and relevant to more people. This is particularly important when Alzheimer’s report ‘Fix Dementia Care: Hospitals’ reports that at least 25% of hospital beds are occupied by someone with dementia ,that they stay twice as long as other people over 65 and the experience of being in hospital is recognised as being a particularly frightening and confusing time.
What have we done ?
We have created an alternative picture story space on the Care Opinion website that is adapted from the work of Talking Mats. The picture story sets were made up after thinking about the topics that arose on the care opinion website .Then we worked with our expert advisor groups which included
- people with dementia,
- their carers
- staff
Our aim was to find a structure that would be comprehensive whilst keeping thing simple and not overwhelming .After a period of consultation and trialling the sets with people with dementia and their carers we have ended up with two sets one that covers the ‘environment’ and one that covers ‘care’
Who can use this and what support will they need?
We know people with dementia have a very diverse range of needs and that people will require different levels of support to give their feedback on the care opinion site ranging from technical support, scribing, to reducing number of pictures, to pre-preparation using paper pictures. Some people with later stage dementia may find it hard to use it to give their own feedback but hopefully, the pictures will mean that they will still be involved and understand some of the things being talked about if people are submitting feedback on their behalf.
We felt important that that the picture story space is an inclusive feature available to all to use if they want to. Whilst this feature was designed for people with dementia we have already had feedback that other people are finding it helpful.
The Picture Stories and Talking Mats
Several people have asked us if this is a Talking Mat and our response is that it is inspired by our work but it is different and for that reason we call it a ‘picture supported story’ .It is different partly, for technical reasons but also because the contexts in which people choose to give feedback will be varied e.g. some will do it by themselves, some supported by family and friends. Above all we want this to be freely available and recognise that that means people will use it in a variety of different ways some of which will surprise us!
We are still developing support materials and webinars to go along with the site to help people get the most from it.
However, there will be some people particular those with more severe communication difficulties who will need increased support to access the story space. Effectiveness for this group will improve if there is some preparation work to prepare their feedback .Using the paper set combined with the principles of Talking Mats to support communication will help. It is for this type of support we recommend attending a Talking Mats foundation training so people are confident and skilled using the pictures in a Talking Mats framework.
Soft Launch
For the last month the picture story feature has been available on the site and we are starting to get a range of stories on it. I particularly like the one that was submitted by a school pupil on work experience supporting a person with dementia to share his experience of going to an inter-generational quiz at the local nursery which had been a very positive experience for all involved.
So please give the site a go, submit your stories or encourage others to use it and please tell us how you got on. Click here to start
We’re always amazed to hear from people about the variety of topics they cover using Talking Mats –from how someone is managing their self care or domestic tasks, to arranging a wedding, or thinking about whats important at a funeral.
As a communication tool Talking Mats maximises a person’s capacity to reflect on a topic and express their view. It gives confidence in decision making.
Here are some other topics we’ve heard about recently.
- As a conversation tool in class
- Pupil voice in school improvement plan
- Client contribution to meetings and review day placement
- Respite
- Operations e.g. gastrostomy
- Health
- Postural management
- Where to live
- Childs opinions in relation to GIRFEC
- Respite feedback/choices
- SW assessments
- Choices available within service
- Going somewhere new
- Transitions
- Problem solving ie horse riding, identifying the problem
- Eating and Drinking
- Keeping Safe
- Social Media
What do you want to talk about? There is no limit!
 Online training login
Online training login