It is recognised that it is difficult for people with communication disability to give feedback to health service staff. The group that developed the Making communication even better resource decided that mystery shopping would be a good way to find out whether health staff were supporting their communication and enabling them to access the services that they require and are entitled to. Funding was sought and gained from NHS Education Scotland for a small mystery shopping project.
20 people with communication disability were involved in the project which was coordinated by Talking Mats Limited and the Stroke Association Scotland. There were different aspects of the project – making phone calls, face to face visits and recounting personal experience . It covered the 14 Health boards in Scotland. The project report was named ‘Through a Different Door’ as this reflected the overall findings that people had highly varied experiences of interactions with health service staff ranging from the excellent and supportive to poor which had the further risk of endangering patient safety . Click here to read the final reports
Whilst developing the eating and drinking resource, we tried it out with people with a range of eating and drinking difficulties. I talked to Ellie, who had swallowing difficulties following a stroke. She found it really helpful to use the mats to think about different aspects of meals (mealtimes, where you eat and the process of eating). Ellie had very good insight into her eating and drinking difficulties and had developed clear strategies to help manage them. She found breakfast and snacks the most difficult meals to manage. She was also very clear that pureed and soft moist foods were the safest and easiest for her. After we had done the mat, Ellie reflected on her eating and drinking, saying that it was limiting but that she could see that things had improved. One of the most difficult things for her was the impact of her swallowing difficulties on some of the social aspects of eating. She really misses going out for a meal with family and friends, something that we often take for granted.
Doing the ‘meals’ mat helped Ellie to see that although she still has many difficulties, mealtimes have become less stressful. For example, although eating and drinking is still a long, slow process, Ellie and her family have adapted to this and now manage ok, especially if they plan ahead. Some useful action points were also identified for the professionals working with Ellie – it would be good for her to have suggestions about a greater range of breakfast options as well as a variety of snacks which she could eat between meals.
Using the mats really helped to clarify the progress that Ellie has made with her eating and drinking since her stroke.
We are launching our fantastic eating and drinking resource to support shared decision making. This has been co-produced with the help of people with eating and drinking difficulties and a range of different professionals. The resource is designed to help people think about, discuss and make informed decisions about how to manage their eating and drinking more safely. People with eating and drinking difficulties should initially be assessed by a qualified Speech and Language Therapist and Dietitian who will recommend appropriate strategies to help them eat and drink safely. This resource is particularly useful in helping people understand the effect that their eating and drinking difficulties can have on their health. It also helps people talk about how they feel about recommended strategies.
When discussing eating and drinking, there are many issues to consider. We have provided symbols under three main topics to help present ideas in a structured way that reduces the likelihood that the person will be influenced.
Click on this image to see it more clearly.
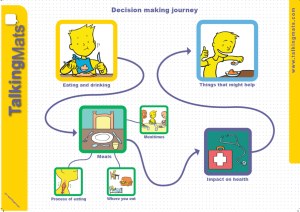
Discussing these topics separately means that people can firstly consider how they feel about different meal times, where they eat and types of food and then think about the impact that their eating and drinking has on their health. It also allows people to have a conversation about some of the suggested strategies and how acceptable these are.
Thanks to Lauren Pettit for this thought provoking blog about using Talking Mats in a rehabilitation setting in South Africa to compare goals of adults with aphasia, their Speech and Language Therapists and their significant others.
I am a Speech-Language Therapist in Johannesburg, South Africa and I work in neuro rehabilitation for people who have had a stroke or head injury. Over the past few years, I have been inspired to learn more about implementing communication modes to assist people to participate effectively in various communication interactions.
Talking Mats™ is such a wonderful tool that enables people to communicate so many things, from their needs and desires, to engaging in higher level conversations. I have seen the benefits of this tool used in a rehabilitative setting. I recently completed my dissertation with the Centre for Augmentative and Alternative Communication (CAAC) at the University of Pretoria, in South Africa.
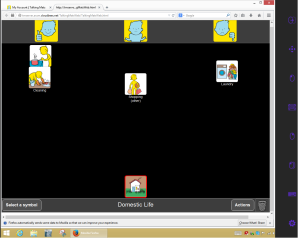
The study included adults with aphasia who were still attending therapy at least 6 months after their stroke and were working on activities and tasks in various therapies, for example: Occupational Therapy, Physiotherapy, Speech-Language Therapy, therapies. I wanted to understand what was important for them to work on in rehabilitation to improve in various areas of life. Some of the adults with aphasia had very little or no speech, others had difficulty expressing themselves and finding the appropriate words to use in a phrase or sentence. Talking Mats™ was therefore used to assist them to rate important life areas. The life areas (activities and participation domains) were identified by the International Classification of Functioning, Health and Disability (ICF). This classification system was created by the World Health Organisation (WHO) and may guide therapy assessment and management. The areas were depicted as symbols with a supplemented written word on each card. These nine cards were: Domestic Life, Relationships, Work and Education, Leisure or Spare time, Self Care, Learning and Thinking, Coping, Communication, and Mobility. The adults with aphasia were asked what was important to them to work on in rehabilitation. The adult with aphasia could place the card under Yes, Maybe or No on the velcro mat and provide a comment if he/she wished or was able to. The Speech-Language Therapists who worked with the adults with aphasia and their significant others (a family member/friend or carer, who knew the person well) were also included in the study. They were asked to identify which areas they thought were important for the adult with aphasia to still work on in therapy.
(Click on graphs to see clearly)
It was very interesting to see varied opinions in the results. Six of the areas received similar ratings from all the participants and Communication was highlighted as an important area to work on by all. There were statistical differences found for the following domains: Work and Education, Leisure or spare time and Self Care. The adults with aphasia wanted to work on Leisure or Spare time and Self Care, however, Work and Education was not important to them to work on in rehabilitation, whereas the Speech-Language Therapists rated Work and Education as important for the adults with aphasia to work on. Significant others did not rate these domains as important.
This study gave a glimpse into how some rehabilitation teams are currently communicating and working together and that very often, the people who have difficulties expressing themselves are perhaps not always given the time and space to understand the therapy plan and identify and communicate their individual therapy needs. This needs to be explored further. Talking Mats™ provided a structure and gave the adults with aphasia a ‘voice’ and the opportunity to engage in this complex communicative interaction. I am in the process of sharing the results from the study with the participants. I have encouraged them to sit together in their teams and identify areas that could currently be focussed on in their therapy. Many participants were eager to discuss the results after the interviews were conducted and were interested in the concept of prioritising their rehabilitation needs. I hope they see their participation in this study as the opportunity to further engage in their rehabilitation needs and that it gives them the confidence to participate more fully in many other areas of their lives that they identified as important.
I would so appreciate your thoughts and input. Please respond to Lauren lolpettit@gmail.com
We’re delighted that Andrea Powell, an Occupational therapist in Edinburgh has written a Blog for us about her experiences of being involved in group work with people who use AAC.
As a student occupational therapist, I worked part time as a support worker with an amazing lady Jennifer, (Jennifer is a pseudonym) Jennifer just happened to use an iPad to communicate. At this time I was about to commence my final year studies and was required to research and write a dissertation on a subject of interest. The lightning bolt of inspiration came when I, with Jennifer attended a weekly AAC user support group which was run and organised by a group of SLT’s.
The group was a wonderful resource that truly benefited the people who used it. I witnessed how much Jennifer valued spending time chatting with friends who also used an AAC device and who understood the unwritten rules of engagement. Such as patience while I set up my speech, don’t look at my screen while decide what I want to say etc. Her confidence in using different types of conversation grew while attending the group. It encouraged her to add to her already wide and variety vocabulary. As her support worker I also valued the opportunity to gain access to training on how to use her AAC and how I could provide better support to her.
I began reading around AAC and how people integrate of devices into their lives. I was however shocked to find that the wonderful group Jennifer attended was a rare occurrence for many users. The more I read, the more I realised that many users struggled to continue using an AAC device due to lack of support, access to trained professionals and most did not have wonderful resources like user support groups.
As an OT I was interested to explore the role in which I would play within AAC provision and found that as an OT I would be mainly providing support and advice on positioning, accessing devices and ergonomic type support.
However I felt that as an OT we have many more skills that didn’t appear to be to be getting utilised, within in my dissertation proposal I postulated that OT’s could expand their role within AAC to i) collaborating on assessments for AAC; ii) training on devices once they have been issued to users; and, iii) running and facilitating groups for AAC users and communications partners in the community.
OT’s are highly trained specialists skilled at understanding what is achievable and realistic for an individual. Occupational therapists assess individuals holistically in order to establish realistic and manageable goals which can be graded and adapted to suit the individual. Through the utilisation of appropriate grading of an occupation, a user can experience success and therefore less failure and frustration, ensuring the challenge is set at the appropriate level for the individual concerned (Park 2009).
Running and facilitating groups as a therapeutic tool is something that occupational therapists have been doing since the earliest days of the profession and groups are now utilised in many areas of practice (Howe and Schwartzberg 2001). By continuing this tradition, occupational therapists are well placed to take the lead in running and facilitating groups for AAC users, integrating social and community activities into the groups, for example, meeting in local shops to provide real life experience of interactions and, importantly, promoting the use of AAC to the general public. There are similar projects being attempted in Motherwell to increase the awareness of Dementia and make local businesses “Dementia friendly” (Shafii and Crockett 2013). Providing groups for AAC users not only enables them to learn how to use their devices, but also provides a support network of other users and communication partners.
I feel that if the skills of an OT were utilised in more than ergonomics then more positive outcomes could be seen for the user of AAC. I believe that if there were more OT’s taking on additional roles within AAC provision it could help reduce the pressure for SLT’s and the waiting lists to see SLT’s. It would also enable more users to be assessed to use AAC.
Many thanks to Helen Paterson, one of our accredited trainers for this fascinating blog.
Now that Talking Mats is accessible in a digital format, the Talking Mats team are often asked ‘Can it be used on an eye gaze device?’ . Of course, for those who use eye pointing reliably, they can use a standard Talking Mat, but there are those individuals with whom we work with who may want to use their eye gaze device to use a Talking Mat, and who find the digital format more accessible. We would suggest that this is only done with a client who is already familiar with eye gaze , due to the extra effort required both to use eye gaze and to make decisions when using a mat. There are many other access methods with which you could use and access Talking Mats Pro, such as a head mouse, chin joystick or touch screen, but for this blog we will focus upon eye gaze. Here’s how we made it possible, and I am sure there may be other ways which we would love to hear about!
- To use Talking Mats Pro directly using eye gaze the person really needs to be calibrated on a device, and they require a level of calibration that is good enough that they are able to access a mouse emulator or Gaze selection on Tobii.
- You must ensure that the mouse emulation or Gaze selection features are set up and the person understands what the features are and what they mean e.g: left click, drag and double click.
- Open up Talking Mats pro on your account.
- You will need to select the topic, topscales and symbols for your client, as this will make it easier with less work for your client, although this is something you would do anyway as the person facilitating the mat.
- Now go through the question and the topscales as you usually would and explain them to your client.
- Select the first symbol and place it on the mat where they can see it.
This is where the 2 systems differ:
Mouse emulation: 
- Client first needs to open the mouse function menu by fixing his or her gaze on the small grey icon which will open the mouse menu.
- Client then fixates gaze to select the drag function (shown above)
- Then the client will select the symbol s/he wants to move by fixating on it.
- Once fixated, they symbol will ‘drag’ around the screen with the clients gaze. 5
- They will then fixate on a point to ‘drop’ it.
See Video
Gaze selection (Tobii):
- The client clicks selects drag function at the top of the Menu
- They then look at the symbol 3
- They then look where they wish to place the symbol.
This does require some more thinking on the side of the client as they need to look to where they want it to go and they are not just dragging it as they are in mouse emulation mode.
See video
For individuals who do not have a calibration good enough to use mouse emulation or gaze selection, it is a little more complex. A Talking Mat could be emulated from software such as The Grid 2 or Communicator, but it would not involve the software from Talking Mats Pro or dragging of symbols and moving them to where the person wants them to go.
Thanks to Andrea McQueen from Australia for this lovely blog describing the Good Things Project which shows how good communication is central to active participation for people with intellectual disabilities
Across the world, many thousands of people with intellectual disabilities live in group homes. These are houses in the community shared by about four to six people with disabilities. Many of these people have communication difficulties of various sorts.
Communication is essential to many activities both within the home (e.g. making a shopping list, choosing what to watch on TV, letting your house mates know when you need some space) and beyond (e.g. developing and maintaining friendships; participation in education, employment and leisure). For many group home residents, participation in these activities relies on access to appropriate augmentative communication systems, and to trained staff who can support their use.
In twenty years working as a speech pathologist in Australia I have been in and out of a lot of group homes. Some do things better than others. Some value communication more than others. Some group home staff routinely use augmentative communication systems, such as Talking Mats, Key Word Sign and pictorial timetables. Unfortunately many do not. Each time I leave a group home, I ask myself the same question: “Could I live here?”
When I first came across the Roydon Street group home here in Melbourne I was impressed. This is a house where communication is respected, where people are listened to, and where genuine choices are offered. It’s not perfect, but it passes my simple test – it is a place where I could imagine living a good life.
I wanted to share the philosophies and practices of Roydon Street around the world. I hoped to influence other group homes to adopt the same simple strategies for their residents. So I sought funding and made a video – Good Things.
The Good Things video aims to show how simple communication strategies can contribute to a good quality of life for people with intellectual disabilities in group homes. It demonstrates how a culture of respect and autonomy can develop when staff understand how to listen to clients and support their communication methods. It shows what is possible in a sector that gets a lot of negative publicity.
Good Things was funded by the Victorian Department of Human Services, and the closed captions on the video were funded by the City of Bayside. The video is the result of a partnership of many agencies and individuals. Special thanks to the residents and staff at Roydon Street. Good Things was released on YouTube in March 2014, and to date has had more than 800 views in 17 countries (not quite keeping pace with Lady Gaga!). It’s a small project, but I hope it has made a difference. I know the team at Talking Mats shares the passion for improving the lives of people wherever they live, and I would love to hear from others with an interest in this area.
Click here to see the Good Things video
Andrea McQueen
Inner South Communication Service
Email: amcqueen@cbchs.org.au
Twitter: @aj_mcq
We are delighted with the response to our new Talking Mats symbols. They created a real buzz at the ISAAC (International Society of Augmentative and Alternative Communication) Conference in Lisbon last week.” Its so good to see something fresh and engaging” , “These are awesome”
Over the past few years we have been looking at symbols in a new way and have used our specialist skills from clinical practice, research and language structure to underpin their development. These skills, in partnership with a leading comic artist, www.adammurphy.com , have enabled us to design our symbols, making sure that they are:
- Unique
- Attractive and fun
- Simple but represent concepts clearly
- Distinguish between concrete and abstract concepts
- Show full body, not stick figures
- Acceptable in terms of age and ethnicity
- Balanced between male and female
- Provide additional visual clues within topics to support understanding
Talking Mats does not require people to select and ‘name’ symbols – the important feature is that the symbols act as a support to hang meaning on. In this way people can understand and use the symbols to express their views .
To determine the size and colour of the symbols, we have used a pragmatic approach as follows:
A search of the literature showed that very little empirical research has been written about optimal symbol size and colour for different client groups. However several leading graphic and cartoon designers use yellow as this is easily recognisable, attractive and ethnically neutral e.g. Simpsons, Lego
- Our artist advised us that cool colours such as blue recede into the background visually whereas warm colours such as yellow stand out more
- We believe it is important to include text as this provides additional input for many people e.g. many people with dementia can read.
- From discussion with colleagues and reading learning disability literature we decided that Arial, san serif point 14 would be the clearest font
- We experimented with various sizes, using very large symbols on one dementia project. However we found that very large symbols are too distracting and limit the number of symbols that can be used on a mat. Following piloting with older people in care homes we determined that the optimal size for using with Talking Mats is 5.5 square cm.
- We ran focus group discussions with speech and language therapists, people with learning disability, people with aphasia and people with dementia. The focus groups presented participants with symbols of different styles, size and colours. The resulting responses plus our literature search led us to the current symbols in terms of design, size and colour.
- We then piloted the symbols in several settings including a day centre with adults with complex physical and cognitive disabilities, a care home with people with dementia and a secondary school with children with additional support needs. In all of these setting almost all participants were able to see, recognise and use the symbols appropriately.
- We made a conscious decision not use photos because photos often have too much detail on the one hand or conversely can be too specific… but that’s a topic for another blog!
We are constantly extending the range of symbols and are currently working on a resource for helping people to consider their Eating and Drinking. We are also working on providing additional visual clues within topics to help people understand concept more easily e.g. emotions are represented within a cloud border. e.g this poor guy is feeling guilty
We are really excited that our new symbols are now being used by 2 organisations outside the field of disability to help students and graduates reflect on their skills,strengths and weaknesses.
For further information click here
Angela is a speech and language therapist in Northern Ireland where she works with people with learning disabilities. She worked with John who had some difficulties with eating and drinking. Together they used Talking Mats to help John understand his risk of choking and identify foods which were easy or difficult to eat. Watch this film clip where John describes how Talking Mats helped him to understand and manage his risk of choking.
My name is Karin Torgny, I’m from Sweden. My background is in journalism and culture studies. I used to work in “The Development Centre for Double Exposure” for many years, and our mission was to improve and spread knowledge about violence against women with disabilities. My special interest during these years was AAC. Today I work for Unicef and in different projects on human rights issues.
A year ago I did my accredited Talking Mats training in Stirling, Scotland. Since then I have given my first course in using Talking Mats when talking about abuse and harm. It was a great experience and an opportunity to work with an enthusiastic group of women who were open and willing to communicate using symbols. They are all in an organisation working with girls/women with intellectual disability exposed to violence and oppression in the name of honour.
I think Talking Mats is a good tool when approaching difficult subjects and I hope to run more courses like this in Sweden in the future. Lately I was interviewed on the Swedish Radio and talked about the use and possibilities with Talking Mats when someone is exposed to harm and abuse.
For those who know Swedish (!), here is a link to that program, http://t.sr.se/1mxZv9W
I am also curious if someone else is doing something similar. If so I would be interested to know more. Send an e-mail to: karin.torgny@gmail.com
Have a look at how Talking Mats has been used in Scotland to support people with a learning disability to disclose issues of concern: Survivor Scotland
 Online training login
Online training login