We are very grateful to Marieke Lindenschot from the Netherlands for this great blog about finding out what activities children like and we look forward to hearing the next stage of her PhD.
For my PhD research in the Netherlands I use Talking Mats as a tool for my interviews with children. The children I interview vary in their communication abilities. Some are able to express their opinions and feelings very well, others are not able to communicate orally. As I was able to purchase the Talking Mats cards without text, I wrote down the words in Dutch in ‘children’s language’ on the cards.
Last week was an exciting week. I conducted the first pilot interviews with a boy of 12 years, a boy of 9 years and a girl of 8 years. They varied in their development. The first interview went great. The child could express which activities he liked, which he disliked and which were ‘so, so’ (in between like and dislike). With Talking Mats he could also tell me with whom he performed the activities and where. It was a fun way to get a lot of information in only 15 minutes! The child and his mother were very enthusiastic. He was able to tell a lot more then he usually does when he is asked about his activities! Unfortunately the other two interviews didn’t produce the same amount of information. The cognitive level of these children seemed too low to use Talking Mats. The boy didn’t understand the top scale ‘like’ and ‘dislike’, whereas the girl didn’t recognize the activities on the cards.
Overall we were very satisfied with these pilot interviews. The goal was to check if the interview guide with Talking Mats ‘worked’ and also to see for which developmental level this way of interviewing is possible. The pilot interviews gave a lot of information on these two goals. I am looking forward to the next interviews as Talking Mats showed to be a very helpful tool in finding out which activities children like.
Please send us any other examples of how you have used Talking Mats.
Laura, shares a story from a speech and language therapy colleague. Her 4 year old daughter was getting upset at the thought of going to nursery; she wanted to see if using a Talking Mat might shed some light on why she was upset as the reasons were unclear.
Topic: Nursery
Top Scale: Like/ Don’t know/ Don’t Like
Options: 14 in total, focusing on different aspects of Nursery involving staff, other children, activities and environment.
The parent reports that her child was very engaged when doing the Mat, and took the photo of her completed mat at the end. Mum took the role of the ‘Listener’ however Dad was also there watching, so the child had the attention of both her parents.
The completed mat indicated that the child liked a number of aspects about nursery, however did not like ‘smell’, ‘sound’ and playing games with other children outside. The parent then fed this information back to nursery staff who are now monitoring these areas in order to gain further information.
This further information from staff will help to provide ideas regarding possible options to sub-mat in the future, using the topics of ‘smell’, ‘sound’ and ‘playing outside’, and therefore enabling this child to communicate her feelings about these areas in more detail.
Those of us who are parents can find ourselves in the position of trying to work out why our child is behaving in a certain way. Sometimes a change in behaviour can be very sudden. Often the underlying reason can be far removed from what we assume it is.
Talking Mats can help in this situation, as it provides a visual, picture-based framework to focus on, supporting discussion between parent and child. Children will often share more information using a Talking Mat as opposed to a purely verbal discussion. Talking Mats is less confrontational and puts the child in control, as the ‘Thinker’.
Health professionals from Stockport have shared how using Talking Mats has positively impacted on their clinical work.
Laura, our North West Associate, met up with Carla Innes, Clinical Psychologist for learning disability from Healthy Young minds Stockport (a child and adolescent mental health service provided by Pennine Care NHS Foundation Trust) and Clare Royle, Family Support Worker,from the Children’s Learning Disability Team (provided by Stockport NHS Foundation Trust). The two organisations work closely together to provide joined up care to young people with a learning disability.
Six months ago Carla, Clare and seven others from the Healthy Young Minds Stockport Team received training to enable them to introduce Talking Mats as part of their challenging behaviour pathway.
Carla and Claire said that the staff team are very positive about the impact of Talking Mats. The overall impression is that Talking Mats has enabled staff to gain an individualised sense of the child or young person they are working with, as well as empowering the children and young people to share their views and opinions. Carla also notes that using Talking Mats has helped her to focus on the child/young person’s abilities/potential – their ‘zone of proximal development’ – and to ensure that everyone is working within that.
Some of the other positive features of using Talking Mats include:
– Providing ‘headspace’ for the child/young person to process their thoughts and to really consider what is important to them.
– Giving a holistic, child/YP centred account and narrative of their feelings and behaviour.
– Helping to inform and direct clinical decision making e.g. introduction of an approach such as CBT.
– Enabling children/young people who have previously refused, or been very reluctant, to share their views and opinions about topics which have been troubling them for example, school attendance and issues with sleep.
– Providing of a communication framework which is neutral and non-threatening – much less intense than direct verbal questioning or conversation.
– Helping to make abstract concepts more concrete for the listener to understand.
– Being a safe, flexible and quick method of finding practical solutions and determining direct actions.
– Enabling the listener to gain a better understanding of the thinker’s level of knowledge and understanding about a particular topic such as healthy eating. This can help inform capacity assessments e.g. in terms of medical consent or the use of medication. The mental capacity act states that appropriate support should be given to young people to make informed decisions and to communicate those decisions.
In addition, from a wider team perspective, Carla and Clare report that they have all noticed benefits in terms of consistency of Talking Mats use by all members of the multi-disciplinary team. Each team member using the Talking Mats tool is working from a slightly different perspective; using Talking Mats ensures that the child/young person is kept at the centre of the process. This results in a truly holistic view of the child/young person’s feelings, views and opinions.
Many thanks to Nicola Lewis from London who has sent us this powerful blog. She has 2 roles – one as a Registered Intermediary with adults with learning disabilities and the other as a family mediator working with children.
I started work as an intermediary, assisting vulnerable people to communicate their evidence to the police and in court. I work with adults with a mild to moderate learning disabilities or mental health issues and with children. The Talking Mats tool has proved invaluable, initially as a rapport building exercise which enables me to build a connection with the person. At the same time I can assess their communication in an informal way. I notice that it is often a relief for those who don’t want to talk as they can just engage in moving the pictures around, without having to make eye contact or without having to speak.They do often start chatting, in spite of themselves as there are not many people who don’t like to talk about their likes, dislikes and preferences and to be heard about what is important to them. I use active listening: reflecting back what they say, summarising, reframing and a touch of humour if appropriate to build a connection, using the mat. When they see me the next time, they often remember me in connection with the Talking Mat:”oh yeah, we did that picture thing!”
I also work as a family mediator and have a specialist qualification enabling me to meet with the children of the family to discuss their wishes and feelings. Again, the Talking Mats tool is the first thing out of my bag and on the table. After working through likes and dislikes in a natural and informal way, I can then use the cards with the children and ask about “your family”, “where you live” etc to find out about how they are managing in a divorce situation and what they might want their parents to know about their feelings. Many mediators will only meet with older children. The Talking Mats tool has given me access to the thoughts of those as young as 5. They are at ease with me and there is a level of trust that did not exist when they entered the room.I have had 100% positive feedback from these meetings as a result.
Thanks for developing this amazing tool. It is incredibly useful to me in both my roles.
Please send us any other stories you would like to share
Many thanks to Greg Cigan for this great blog about his study that explored how children and young people with an intellectual disability feel about undergoing clinical procedures.
A clinical procedure is any activity performed by a healthcare practitioner to diagnose, monitor and/or treat an illness such as blood pressure testing, x-rays and other scans (Cigan et al., 2016). While some procedures cause no pain or only mild discomfort when completed, others can be prolonged and potentially painful (Coyne and Scott, 2014). Children and young people with an intellectual disability are more likely to develop physical illnesses including epilepsy and digestive disorders than the general population and can be frequently required to undergo healthcare procedures (Emerson et al., 2011; Short and Calder, 2013). Yet, there is currently little empirical research reporting how children and young people with an intellectual disability experience procedures (Peninsula Cerebra Research Unit, 2016). More research is required so that healthcare services can better understand the needs of children and young people with an intellectual disability (Oulton et al., 2016). As part of my doctoral studies at Edge Hill University, I am conducting a study that explores how children and young people with an intellectual disability experience having a clinical procedure.
From the outset of the study, I felt it was important to obtain data directly from children and young people rather than relying on parents and carers to speak on their behalf. I was keen to adopt methods during interviews that would enable as many children and young people as possible to take part, including those who find verbal communication challenging. After researching different methods, I chose to utilise Talking Mats as the innovative design of the tool offered children and young people the option to express their views entirely non-verbally should they wish to by arranging symbol cards. To date, I have interviewed 11 children and young people about their experiences of undergoing procedures. Each participant was between 7-15 years of age at the time of the interview and had a mild to moderate intellectual disability.
Prior to an interview beginning, I spent time describing and showing each child/young person a Talking Mat and asked whether they would like to use the tool during their interview. Out of the 11 children and young people I have interviewed, three used a Talking Mat. Those that chose not to use the tool were older children who were confident having a verbal conversation with me or those who had a visual disability and could not see the symbols. In all cases, the decision of the child/young person in relation to using the Talking Mats was respected.
The three children who used the Talking Mats were able to express their views non-verbally and also seemed to convey more information than some of those who chose not to use the tool. Viewing the symbol cards within a Talking Mat appeared to help children and young people break down information into smaller chunks which then made it easier for them to process and discuss. Indeed, using a Talking Mat led all three children to discuss information that was new to their parents who sat in while s/he was being interviewed. An example of a completed Talking Mat is shown below which was created by an 11-year-old boy during his interview. The boy clearly expressed that he did not enjoy his experience of having a clinical procedure.
Within my study, I feel using Talking Mats has helped to augment the verbal communication of some of the children and young people which in turn enabled them to take part in interviews and share their views and experiences of procedures. Talking Mats are a valuable tool for researchers working within the field of intellectual disabilities. If used more widely, Talking Mats has the potential to enable more children and young people with intellectual disabilities to have the opportunity to be involved and express their views within healthcare research.
Reference List
CIGAN, G., BRAY, L., JACK, B. A. and KAEHNE, A., 2016. “It Was Kind of Scary”: The Experiences of Children and Young People with an Intellectual Disability of Undergoing Clinical Procedures in Healthcare Settings. Poster Presented at the 16th Seattle Club Conference (Awarded Best Poster Prize), 12-13 December. Glasgow: Glasgow Caledonian University.
COYNE, I. and SCOTT, P., 2014. Alternatives to Restraining Children for Clinical Procedures. Nursing Children and Young People, 26(2), pp. 22-27.
EMERSON, E., BAINES, S., ALLERTON, L. and WELCH, V., 2011. Health Inequalities and People with Learning Disabilities in the UK: 2011. Lancaster: Improving Health and Lives: Learning Disabilities Observatory.
PENINSULA CEREBRA RESEARCH UNIT, 2016. What’s the Evidence? Reducing Distress & Improving Cooperation with Invasive Medical Procedures for Children with Neurodisability. Exeter: University of Exeter.
SHORT, J. A. and CALDER, A., 2013. Anaesthesia for Children with Special Needs, Including Autistic Spectrum Disorder. Continuing Education in Anaesthesia, Critical Care & Pain, 13(4), pp. 107-112.
If you would like more information about Greg’s work you can contact him at Cigang@edgehill.ac.uk
Exploring sibling attitudes towards participation when the younger sibling has a severe speech and language disability
We were delighted to receive this publication from a friend and colleague, Prof Juan Bornman from Pretoria in South Africa. It reports on a study carried out with 27 typically developing children who have a younger sibling with a severe speech and language disability. Juan and her colleagues used Talking Mats to carried out an adapted structured interview to find out the views of these children on four everyday life situations identified by the WHO-ICF-CY (World Health Organisation’s International Classification of Functioning, Disability and Health, Children and Youth Version).
The four topics were:
Communication
Domestic life
Interpersonal interaction and relationships
Major life areas.
The findings showed that the children were ‘most positive towards participation in play activities with their sibling with a disability. They were also positive towards participation in household tasks. They were less positive towards communication participation and least positive about participation in interpersonal relationships’.
The following example is taken from Juan’s publication.
The article’s reference is:
Exploring sibling attitudes towards participation when the younger sibling has a severe speech and language disability. M Hansen, M Harty, J Bornman South African Journal of Child Health 2016 Vol. 10 No. 1
To read the full publication with details of the methods used and the results click here sibling-attitudes-2016
Thanks to Laura Holmes for telling us more about the innovative work in Stockport.
As part of an ongoing project, we at NHS Stockport Children’s Speech and Language Therapy Service are introducing the Talking Mats approach to support the children we work with to contribute to their own EHC Planning, enabling them to make their voices heard.
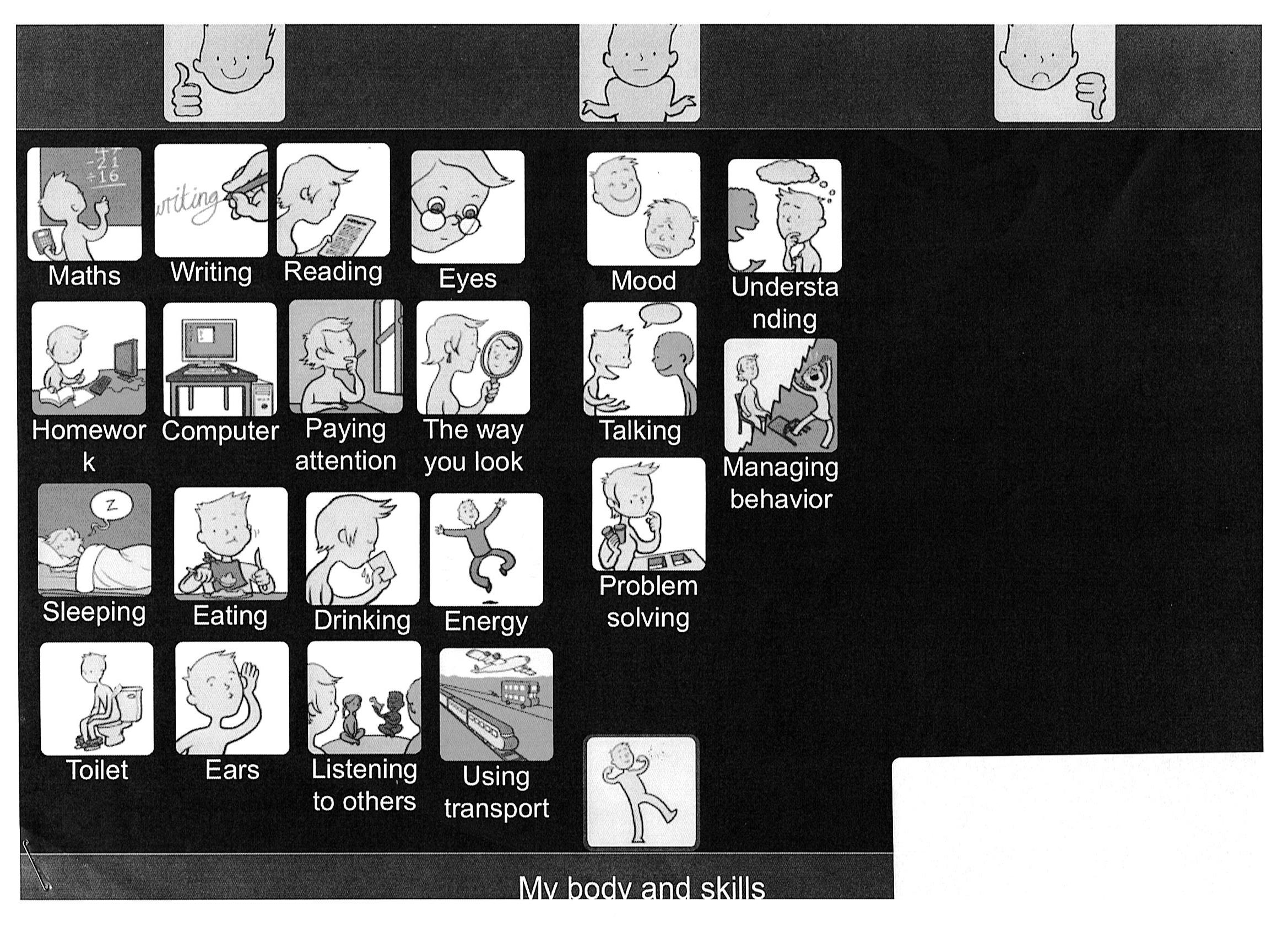
For example, I have used the ‘Consulting Children and Young People – My Body and Skills’ (Primary) digital resource to help identify and plan target areas for an 6 year old child with a diagnosis of Autism. I selected a top scale of ‘happy/unsure/not happy’ and chose a variety of options symbols from the resource. The child (R) was then able to drag and drop each option symbol to the area she felt it belonged in, producing the following talking mat:
Whilst completing the mat the child volunteered further information about particular options – in general I find I get to know the children I work with much quicker using this approach!
Once complete, we agreed that we would sub-mat the option ‘talking’ (which had been placed under ‘unsure’) and explore that option as a topic in our next therapy session.
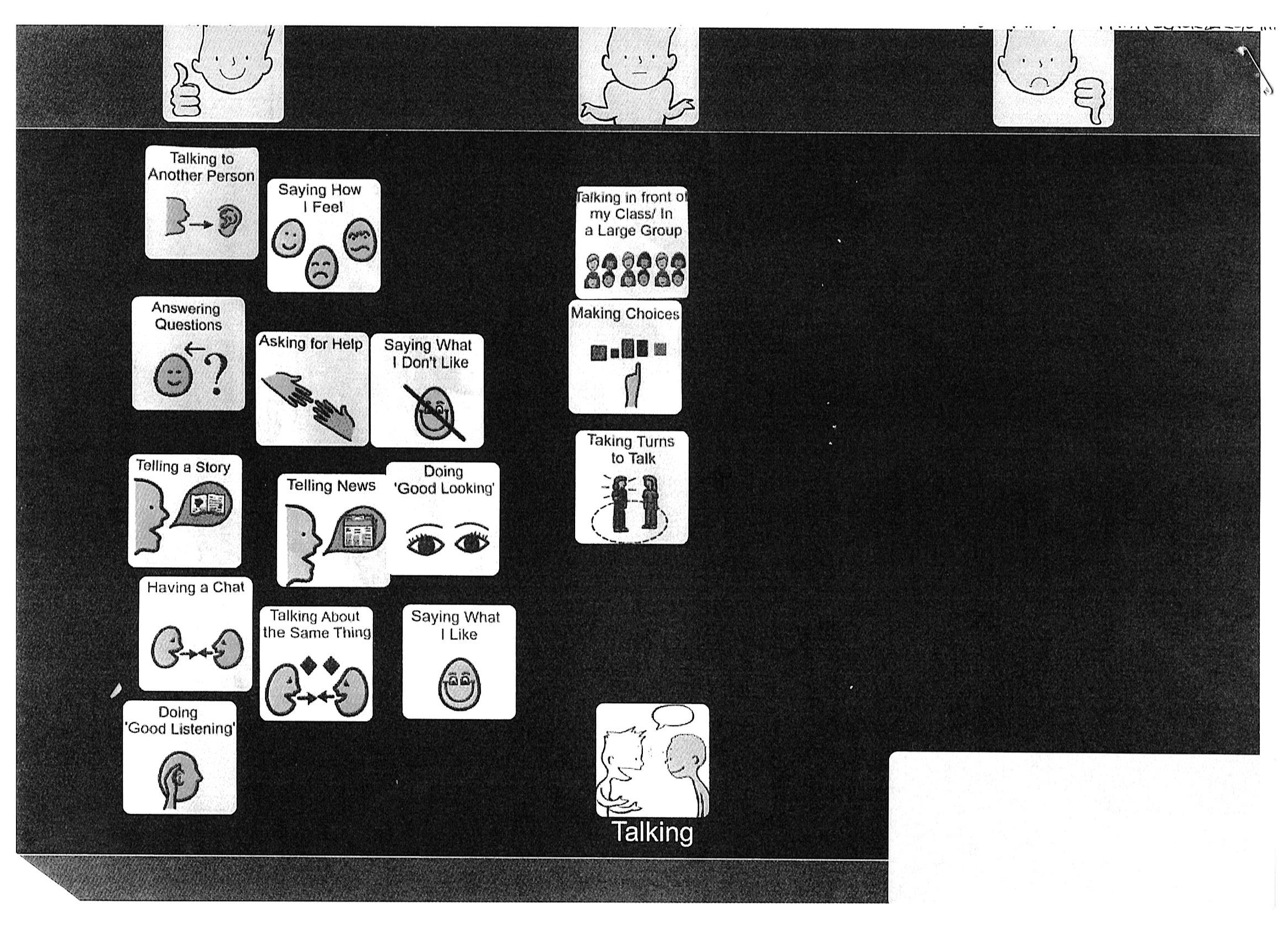
I then thought about all the possible options I wanted to explore in this submat, and created symbols using Boardmaker. I was able to add these symbols as options for the digital mat by taking photos using my Ipad and selecting them from my camera roll.
R completed the submat as follows:
The mat enabled R to pinpoint the areas of talking she feels unsure about – i.e. ‘talking in front of my class/ in a large group’; ‘making choices’; ‘taking turns to talk’. I was then able to include this information in my review report, attaching the pictures of the mats as evidence of consultation. My review report included details of specific targets and recommendations to support R to work on the areas she had identified, which are designed to be incorporated into her EHC Plan.
We know from our own network that many practitioners are looking for training and tools to help implement the SEND reforms. Talking Mats are running a free seminar in Stockport to let practitioners see how Talking Mats can be used. The morning session is FULL but we have added an afternoon session. Book your place now as it is first come first served and places are filling up fast. Free Stockport afternoon seminar
Talking Mats was used as part of a Speech and Language therapy assessment for a boy with a stammer (dysfluent speech). He was very aware of his stammering and would change what he was going to say or avoid some situations because he anticipated that he would stammer. He had low self-esteem about his speech and felt that whenever anyone laughed in his class, it was to do with his stammer.
Talking Mats was used to gather information about which situations and people made speaking easier, and any situations and particular people which caused more of a challenge. The activity provided much more information than originally anticipated.
A starter mat was used to show how a Talking Mat worked, using pictures of food. He engaged well with this, and understood the process quickly. We then moved onto discussing his speech – we wrote names of people in his life and situations which involved speaking onto pieces of paper, and he placed these on the mat where he felt appropriate. We started with people and situations which appeared more positive, then gradually moved onto those it was anticipated would be more challenging.
His insight into his speech and what helped him or made speaking more difficult was impressive. We were able to use this information to compile a list of “Do’s and Don’t’s” for people he came into regular contact with. He agreed that this information could be shared with school to give them strategies to support him there.
The most powerful part of the Mat was him being able to say that he did not feel happy about talking with his big brother sometimes, because he could make fun of his speech, and this made him feel really upset. This was a powerful revelation for his Mum who had sat in on the session, as she had not realised he felt this way. After the session, the family had a chat around the table at tea-time about how his therapy session had gone that day – with Mum’s support he was able to say to his brother about how his teasing had made him feel. His older brother had thought it was all a bit of fun and hadn’t realised the impact it was having. They agreed the older brother wouldn’t tease him anymore.
When he came back for his next session, he commented on being much happier about his talking at home, and felt the activity had been really helpful. His Mum was very positive about it too, and proud of how he had managed to speak up for himself and be able to say how other people could help him with his talking.
Our thanks to Kirsten Taylor, Speech and Language therapist for sharing this powerful story
We are delighted to introduce Laura Holmes our first Regional Talking Mats Associate. She is joining the Talking Mats team and will be working in the North West of England. I will let Laura introduce herself:-
” Hi, I am a Speech and Language Therapist working in Stockport, Cheshire. I am delighted to be joining Talking Mats as the first Regional Associate, covering the North West of England. I work 1 day a week, term-time only for Talking Mats, as well as 3 days a week for the NHS. I am excited about developing awareness, understanding and use of Talking Mats across the area, within the context of the SEND reforms in particular, over the next few months. I feel Talking Mats is a very effective way of truly capturing the voices of the children and young people I work with. The Talking Mats approach also links well with the use of Therapy Outcome Measures, which I am currently trialling with my caseload. I am looking forward to sharing my knowledge and experiences to facilitate wider use of this versatile approach across the North West region.”
It is great to have Laura working with us to build on some of the excellent work being done already in the North West. Two examples of best practice are in Wigan where Talking Mats are used to increase child participation and more recently in Salford. Children’s services in Salford NHS foundation trust are committed to seeking the views of children and young people about how they feel about their health appointments. They have finished piloting their own Talking Mats set and the revised set has just been sent to the printers – it looks great.
We are running a training course in Liverpool on the 21st April and we would love to meet more of you from the North West.
What works well when implementing Talking Mats?
Our last blog highlight how the Wigan Pathfinder Project selected Talking Mats from a range of tools to consult with pupils who have Education, Health and Care plans (EHCP) . They reported that Talking mats provided :
- An objective, neutral space – a thinking tool- ‘Children and young people are able to consider their priorities when setting targets’.
- Opportunities for change – ‘Children and young people are able to make changes to their initial thoughts and have time to decide and reconsider options’.
- A truly person centred approach
- It was fun!
Additional factors they commented on which worked well when consulting with pupils about decision making and goal setting were:
- Good liaison with parents and staff who know the child well before the session
- Adapting the length of the session to the child’s needs
- Ensuring a suitable room without too many distractions
- Using the teaching scale
- Putting the child’s name on the mat
- Placing all topics in one envelope for easy access
- Allowing time to sort symbols and discard irrelevant ones.
- Reducing the number of symbols used depending on the child’s needs
- Changing the top scale symbols to support the child’s understanding where necessary
- Keeping a verbal record where appropriate
- Working in pairs whilst learning the approach
- Using the effectiveness coding framework (all case studies scored above 75%, therefore considered effective using this measure)
The Talking mats training focuses on teaching how to establish a consistent and appropriate top scale, maintaining a clear topic and using the effectiveness framework. It also presents a model for thinking about who can and cannot use the mat and for what types of questions and discussions
 Online training login
Online training login