Many thanks to Ruth Spilman, Senior Speech and Language Therapist, for this great blog about how she uses Talking Mats for Capacity Assessments with People with ASD/LD
I am a speech and language therapist (SLT) working in a residential provision for young people with autism spectrum disorder, learning disabilities and other co-occurring difficulties. We support young people from 7 up to the age of 20. Many of the young people are in a ‘grey area’ with a view to capacity assessments, including those aged 16-18. We support many capacity assessments, including deputy-ship for finances and care, health and welfare, as well as more individualised capacity assessments around restrictions in the environment, consent to medical interventions and making decisions about the future.
A large part of the way we support these capacity assessments is by using Talking Mats, which support people with autism who generally prefer to think about things visually. The young people are encouraged to use Talking Mats in their everyday communication, such as evaluating activities, lessons and therapy sessions to develop their skills, as well as during direct Speech and Language Therapy work. If a young person has proven their competence using a Talking Mat, we can then move on to supporting capacity assessments. As part of the process, the SLT would break down the concepts needed to be understood to identify if the individual has capacity or not. For example with finances, do they know what money is? can they organise things that are expensive and cheap? can they put items in a scale of least to most expensive? This would all be done using a Talking Mat, then followed up if they achieved this task with a range of further activities. A Talking Mat can then support activities to evidence their understanding or lack of, while also giving a young person all practicable help to communicate.
See below two examples of a young person thinking about 1) money to support their finances, and 2) things that are healthy or not.
Talking mats are used for a range of different skills and assessments in the provision I work in, but their use for capacity assessment gives the young people the most practicable support with communication and allows for clear evidence of the person’s understanding of the concepts involved. In addition to the range of items mentioned above, we have have also discussed tattoos, physical intervention and behaviour support strategies, having a lock on an individual’s bedroom door, and understanding of fantasy and reality.
Talking Mats has proved to be a truly simple but brilliant and useful tool.
Ruth Spilman, Senior Speech and Language Therapist, Specialist services in education
The Cambian Group, Dorset, BH19 1PR www.cambiangroup.com
What are the top 10 blogs for using Talking Mats with adults? Over the years we have posted lots of blogs on different aspects of our framework . If you are working with adults with communication disability these blogs maybe particularly helpful
- Where is the best place to start using the Talking Mats health and well-being resource?
- A blog from Denmark which highlights the effectiveness of using Talking Mats with people with dementia
- Goal setting with a woman with Multiple sclerosis
- Using the app with someone with aphasia
- The development of a resource to help people with learning disability raise concerns
- How can Talking Mats support Capacity to make decisions
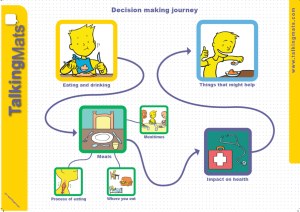
- Involving people in their decisions about eating and drinking
- Thoughts on using Talking Mats with people with dementia to explore mealtimes
- Using Talking Mats with someone with a learning disability and dementia
- Use in a rehab setting in South Africa
If you want to explore our resource and training more please visit our shop
We are very grateful to Anna Volkmer for sending us this blog, Lets Talk about Capacity…
She has just had an excellent book published – Dealing with Capacity and Other Legal Issues with Adults with Acquired Neurological Conditions http://www.jr-press.co.uk/dealing-capacity-legal-issues.html. In it she describes how AAC methods, including Talking Mats, can be used to support people in expressing their decisions.
Prior to 1959 people who were considered “non-compus mentis” were cared for under the “parens patriae” principle. Literally translated this meant that they were ‘parents of the country’ and decisions to protect them and their property were made by the Crown (the Lord Chancellor). These people were often described as “Chancery Lunatics”. In 1959 the “parens patriae” jurisdiction gave way to the Mental Health Act. This Act instructed that “the judge may, with respect to the property and affairs of a patient, do or secure the doing of all such things as appear necessary or expedient…for making provision for other persons or purposes for whom or which the patient might be expected to provide were he not mentally disordered” (section 102 (1)(c)). Unfortunately, this Act did not make adequate provision for non-financial decisions such as medical decisions. During this period it was case law that guided professionals in supporting their patients who lacked capacity in medical decision making. It was not until 2005 that the first Mental Capacity Act was given Royal Assent, accompanied by the Mental Capacity Act Code of Practice in 2007.
I returned to the UK from a 5-year stint working in Melbourne, Australia, just after the Mental Capacity Act had been published. Mental capacity was on the tip of everyone’s tongues and as the speech and language therapist working on a multi-disciplinary team I became an integral part of this process. Patients I was seeing, often people with primary progressive aphasia or other types of dementia, were asking about how to make future decisions. They and their families were keen to understand how the mental capacity act worked, how to prepare for the future and how to have their voices heard. On the other side of the coin I was working on an inpatient ward where staff were concerned about ensuring we were fully assessing the decision making capacity of people with cognitive and communication difficulties, often holding best interest discussion to plan for the future of these individuals. Many of these decisions related to dysphagia, but others related to accommodation and finances.
What concerned me was the lack of evidence available across the speech and language therapy arena in this area. There was little to none in terms of written research, let alone written advice or even examples of good practice tailored to speech and language therapy clinicians. As I asked around I found an enormous disparity in the services that speech and language therapy clinicians were providing across different trusts. I had previously written a book on dementia, and had included a chapter on assessments of decision-making. At this stage some of the only research related to communication and decision-making had come from Talking Mats. This had demonstrated that using the talking mats tools can support families and caregivers in conversations with their loved ones when discussing decisions to be made. They found that conversation enabled people in understanding, retaining and expressing themselves in decision-making discussions.
Following a particular stimulating discussion with the publishers at J&R press, they invited me to submit a book proposal on this topic. As I was developing this idea I found the topic of mental capacity was raised more and more often at study days and seminars I attended. At these study days I started linking in with more like minded speech and language therapists such as Mark Jayes, Hannah Luff and Claire Devereux. These were clinicians who all agreed on the diversity of our potential role in supporting our patients around mental capacity issues. These common interests enabled a collaboration. Our book is now published.
Through these connections I became aware of other work being done; Mark Jayes holds a NIHR doctoral fellowship award and is conducting research in the development of a communication and capacity assessment tool kit. Claire Devereux is the chair of the Southern Psychiatry of Old Age Clinical Excellence Network, together we have held a workshop with the clinical specialists where we developed a consensus document on role of the speech and language therapist in capacity assessment. This is to be published in Bulletin magazine later this year. Hannah Luff is a clinical lead speech and language therapist at South London and the Maudsley NHS Trust and is currently a member of the review panel looking at the NICE SCIE dementia guidelines.
The wonders and value of networking never ceases to delight, enthuse and inspire me! And you can purchase our book at the following website (there is currently a discount rate until 21st February):
http://www.jr-press.co.uk/dealing-capacity-legal-issues.html
You can follow me on my blog https://annavolkmersbigphdadventure.wordpress.com/ or on twitter @volkmer_anna
Following the success of previous seminars we are holding further specialist seminars in Stirling and London for anyone who has done the Talking Mats training. The topics will be:
- Talking Mats and the Eating and Drinking resource (morning)
- Talking Mats and Capacity (afternoon)
During the Eating and Drinking seminar, we provide background on how and why the resource was developed and showed some DVD examples of people using the resource. This really brings things to life and shows how important it is to give people (with and without speech) the opportunity to consider and talk about different aspects of eating and drinking. We also give people hands-on practice in using the symbols from each topic. Each participant will receive a copy of the full Eating and Drinking resource, including symbols, a mat, and explanatory booklet.
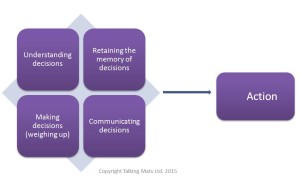
During the Capacity seminar we will discuss the fundamental principles of the Capacity Act and participants will have a chance to consider how Talking Mats can help people to:
- understand
- retain/remember
- weigh up information
- communicate their views/wishes and feelings.
They will also be given the opportunity to work through some practical examples and think about options to help people understand issues and make decisions.
If you have completed a Talking Mats training course and would like to attend either of specialist seminars, please click on the relevant course and fill in the registration form.
Stirling on Friday 29th April Stirling Seminars flier Apr 2016
London on Friday 10th June London Seminars flier June 2016
Registration form Seminar registration form 2016
The inability to make a decision could be because of a learning disability, mental health problems, brain injury, dementia, alcohol or drug misuse, side effects of medical treatment or any other illness or disability. Click here for further information.
Both the Mental Capacity Act (2005) in England and Wales and the Adults with Incapacity Scotland Act (2000) identify the following components which determine whether or not someone has capacity to make their own decisions.
There are a number of additional assumptions that are central to determining whether or not someone has the capacity to make their own decisions:
• Every adult has the right to make decisions unless proved otherwise
• Everyone should be supported to make their own decisions
• People should be given the support they need
• People are entitled to make their decision – good or bad
• Each individual has a different capacity to make decisions about different aspects of their life.
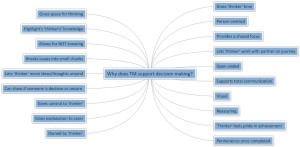
We have been running seminars on how Talking Mats can be used to support a person’s capacity to make decisions.The diagram below illustrates some of the comments we received form participants at a recent seminar about the benefits of using Talking Mats to support decision making.
Click on the diagram to enlarge.
The process of completing a Talking Mat helps people retain their view and if they have memory problems the picture of the mat is a good prompt to enable recall.
Its worth noting that our brain processes visual images 60,000 faster than text!
Recently we delivered two Talking Mats specialist seminars in London:
- Talking Mats and the Eating and Drinking resource
- Talking Mats and Capacity
Both seminars were very well attended with lots of discussion from a wide range of professionals.
During the Eating and Drinking seminar, we provided background on how and why the resource was developed and showed some DVD examples of people using the resource. This really brought things to life and showed how important it is to give people (with and without speech) the opportunity to consider and talk about different aspects of eating and drinking. We also gave people hands-on practice in using the symbols from each topic.
Each participant received a copy of the full resource, including symbols, a mat, and explanatory booklet.
During the Capacity seminar we discussed the fundamental principles the Capacity Act and participants had a chance to consider how Talking Mats can help people to:
- understand
- retain/remember
- weigh up information
- communicate their views/wishes and feelings.
They were also given the opportunity to work through some practical examples and think about options to help people understand issues and make decisions.
If you would like to attend our next specialist seminars, we are holding them in Stirling on 17th February: Stirling Seminars Feb 2015 flier
During a research project funded by the Joseph Rowntree Foundation in 2007, Joan Murphy and Cindy Gray developed the Dementia Communication Difficulties Scale (DCDS) to help identify the communication difficulties that a person with dementia might be having and therefore help carers and staff to understand these difficulties and therefore support the person with dementia. The scale comprises 13 statements that are based on existing definitions of the communication problems commonly experienced by people as dementia progresses (Kempler, 1995; Health Education Board for Scotland, 1996):
In early stage dementia, the person
- may have difficulty coming up with words
- may tend to digress and repeat themselves.
In moderate stage dementia, the person
- may find it hard to understand what is said to them, particularly when being given complex information
- may have difficulty maintaining a conversation topic without losing track
- may use semantically empty words (e.g. thing, stuff) in place of content words
- may be difficult to understand.
In late stage dementia, the person
- may make little sense
- may not be able to understand what is said to them, even when simple language is used
- may often repeat what other people have said to them
- may communicate mainly in non-verbal ways
The DCDS requires a third party who knows the person with dementia well (a paid carer or family member) to assess various aspects of their communication on a 5-option scale. People are asked to circle the option that most closely describes the person in question.
Each DCDS option is assigned a score: for example ‘Never’ = 0, ‘Sometimes’ = 1, ‘Often’ = 2, ‘Always’ or ‘Says too little for me to judge’ = 3. A person’s DCDS rating is obtained by totalling their scores for all 13 statements. DCDS ratings can therefore range from 0-39, with a higher rating indicating a greater degree of communication difficulty.
The following stages of dementia group definitions were produced:
• DCDS ratings between 0 and 10.5 = early stage
• DCDS ratings between 11 and 19.5 = moderate stage
• DCDS rating between 20 and 39= late stage.
The Dementia Communication Difficulties Scale is brief, straightforward and quick to complete, and may therefore provide a highly useful tool for the care staff, clinicians and practitioners involved in assessing the needs of people with dementia.
If you would like a copy of the scale please click here: Dementia Communication Difficulties Scale
References:
Kempler, D. (1995). Language Changes in Dementia of the Alzheimer Type. In R. Lubinski (Ed.), Dementia and Communication, San Diego: Singular Publishing Group.
Health Education Board for Scotland (1996). Coping with Dementia: A Handbook for Carers. HEBS.
Within the Health and Well-being resource there are four symbol sets (health, looking after yourself, communication and leisure & environment). Within the ‘health’ set, there are three topics which can be used to help people express their views about different aspects of their health:
• Health
• Coping
• Mobility
I worked with Pete who had severe aphasia. Pete had a range of health problems, including epilepsy and high blood pressure. Pete found it very difficult to communicate with his GP, and usually relied on his wife to translate. This meant that not all of Pete’s health problems were addressed or discussed when he went to the doctor, and he often felt excluded from conversations at these appointments. Prior to one of Pete’s GP appointments, I used Talking Mats with Pete to find out how he felt about his health. During our discussions, Pete was able to tell me that he was worried about a number of issues, but he especially wanted to talk to his GP about his ears, as he was having a lot of pain and also had a ringing sensation in his ears which meant that he found it very difficult to concentrate, particularly when watching TV.
Pete took the photo of his completed mat with him to his next GP appointment and his GP used this as a focus for discussions. As a result, Pete was referred to an audiologist for assessment. His GP also spent time discussing Pete’s epilepsy with him and referred him back to the epilepsy specialist nurse who worked with Pete and his wife to improve their understanding and management of it.
Using Talking Mats helped Pete prepare for his GP appointment and also ensured that his GP focused on what was important to him. As a result, time was spent more effectively by all and Pete felt listened to and really participated in his GP consultation.
Use the Talking Mats ‘health’ symbols from the health and well-being resource to help people prepare for appointments with health professionals and manage their health more effectively.
The Talking Mats Team is increasingly asked to help ascertain a person’s capacity to express their views from a non-biased perspective. We are also asked to carry out service evaluations and are therefore developing independent consultancies to individuals and organisations. Our team of experienced Speech and Language Therapists, who have an in-depth knowledge of communication difficulties, are well equipped to do this.
The following are examples of independent consultancies which we have been asked to carry out:
- A lawyer asked us to work with a man who had had a severe stroke to ascertain his capacity to make decisions ranging from simple ones such as where he would like to go on holiday to complex ones such as who should control his finances. Using Talking Mats we were able to determine that he could make decisions about simple, concrete situations but wished his wife to make more complex decisions such as finances. check
- A Social Work department asked us to work with a woman with dementia and aphasia who had been sectioned. They needed to ascertain if she could understand why she could no longer live in her own home. We worked closely with her social worker and through using Talking Mats ascertained that she was unable to give informed consent.
- A Health Service facility asked us to evaluate the degree to which their patients felt involved in their care planning.
- A Care Home asked us to use Talking Mats with a 91 year old resident with dementia to find out her views about receiving dental treatment. There had been problems in the past and both the staff and her son were unsure if she understood the reasons and implications for dental treatment. Using Talking Mats, she was able to explain her thoughts about her teeth and dentures and clearly said that she was unhappy about opening her mouth for the dentist but that if her son were with her she would feel much better. We received this comment: “If you were to show the first few minutes without Talking Mats you would have thought this lovely lady lacked capacity, however the change and her engagement is noticeable.”
The following points explain with whom and how we can carry out the Talking Mats consultancy:
- Children or adults
- Family members, friends, professional staff
- Individuals or groups
- With or without a carer present
- At a venue and time which best suits the individual
- On any topic – we already have a comprehensive range of topics for both adults and children – but can create tailored symbol sets for any situation
- To find out someone’s views on a particular topic or situation at a specific point in time
- To help determine the capacity of an individual to make their own decisions
- To compare someone’s views over time
- To compare different people’s views e.g child and parent, person with dementia and carer
- We provide a detailed report with a copy of the person’s completed mat/s
To find out how we can help you and for discussion of costs please contact us at info@talkingmats.com or phone us at 01786 479511
 Online training login
Online training login