During a research project funded by the Joseph Rowntree Foundation in 2007, Joan Murphy and Cindy Gray developed the Dementia Communication Difficulties Scale (DCDS) to help identify the communication difficulties that a person with dementia might be having and therefore help carers and staff to understand these difficulties and therefore support the person with dementia. The scale comprises 13 statements that are based on existing definitions of the communication problems commonly experienced by people as dementia progresses (Kempler, 1995; Health Education Board for Scotland, 1996):
In early stage dementia, the person
- may have difficulty coming up with words
- may tend to digress and repeat themselves.
In moderate stage dementia, the person
- may find it hard to understand what is said to them, particularly when being given complex information
- may have difficulty maintaining a conversation topic without losing track
- may use semantically empty words (e.g. thing, stuff) in place of content words
- may be difficult to understand.
In late stage dementia, the person
- may make little sense
- may not be able to understand what is said to them, even when simple language is used
- may often repeat what other people have said to them
- may communicate mainly in non-verbal ways
The DCDS requires a third party who knows the person with dementia well (a paid carer or family member) to assess various aspects of their communication on a 5-option scale. People are asked to circle the option that most closely describes the person in question.
Each DCDS option is assigned a score: for example ‘Never’ = 0, ‘Sometimes’ = 1, ‘Often’ = 2, ‘Always’ or ‘Says too little for me to judge’ = 3. A person’s DCDS rating is obtained by totalling their scores for all 13 statements. DCDS ratings can therefore range from 0-39, with a higher rating indicating a greater degree of communication difficulty.
The following stages of dementia group definitions were produced:
• DCDS ratings between 0 and 10.5 = early stage
• DCDS ratings between 11 and 19.5 = moderate stage
• DCDS rating between 20 and 39= late stage.
The Dementia Communication Difficulties Scale is brief, straightforward and quick to complete, and may therefore provide a highly useful tool for the care staff, clinicians and practitioners involved in assessing the needs of people with dementia.
If you would like a copy of the scale please click here: Dementia Communication Difficulties Scale
References:
Kempler, D. (1995). Language Changes in Dementia of the Alzheimer Type. In R. Lubinski (Ed.), Dementia and Communication, San Diego: Singular Publishing Group.
Health Education Board for Scotland (1996). Coping with Dementia: A Handbook for Carers. HEBS.
In the Health and Well-being resource, we have provided four sets of symbols to help people consider how they feel about their communication. Because communication is complex and often abstract, it can be particularly difficult for people to express their views about it, especially if they have existing communication difficulties. To make this easier, we have divided communication into four topics:
- Expression
- Understanding
- Learning and thinking
- Relationships.
In the following example, I show how each topic can be used to build up a picture of how someone feels about different aspects of their communication. I worked with Kate, a 42 year old woman who had a stroke which left her with severe expressive and receptive aphasia. She was able to communicate through vocalisations and gestures. She could sometimes draw or write down words and needed to point to ‘yes/no’ in order to reliably answer closed questions. Following discharge from hospital, I used Talking Mats with Kate to find out how she felt about her communication. I started with the ‘communication – expression’ topic and found that she felt that she was having lots of difficulties making herself understood, particularly on the phone and in group situations:
I then explored how Kate felt about understanding what people were saying to her. Kate was able to tell me that she found it easier to understand people on a one to one basis rather than in a group setting. She indicated that it really helped her if people used gestures or wrote things down. Her main difficulty was understanding people on the phone, and in fact she had stopped answering the phone altogether (see mat below).
We went on to do a mat about Kate’s learning and thinking. In this set, there are symbols which cover higher level language activities such as reading, problem solving and organisation. When we talked about these areas, Kate was able to tell me about the things she was finding most problematic, but could also identify some things that she felt she could still manage (such as calculations and reading newspapers).
I then asked Kate how she felt about communicating with different people in her life. This mat shows that Kate found talking to her husband and her parents (who lived quite far away) particularly difficult.
As a result of doing these mats, we were able to target the things that mattered most to Kate in relation to her communication, and came up with the following actions:
1. Kate felt that her husband needed support and information, so we spent time working with him, showing him the best ways to support Kate’s communication.
2. Because Kate’s parents lived quite far away, she could only contact them using the phone, which was very difficult. We worked on getting Skype set up so that Kate could communicate with her family using all the modes available to her.
By splitting communication into different sub mats, Kate was able to think about different aspects of her communication and identify the things that she found most challenging. Together we began to work out some ways to help her overcome her difficulties.
Use the communication symbols to find out what people want to work on and use a collaborative approach to establish some goals to work on in therapy. I used the original Talking Mats when I explored Kate’s communication with her, but you could do the same with Digital Talking Mats. Find out more about it here.
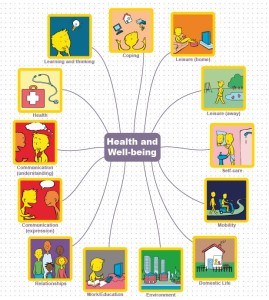
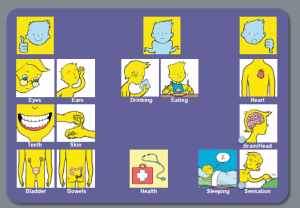
Within the Health and Well-being resource there are four symbol sets (health, looking after yourself, communication and leisure & environment). Within the ‘health’ set, there are three topics which can be used to help people express their views about different aspects of their health:
• Health
• Coping
• Mobility
I worked with Pete who had severe aphasia. Pete had a range of health problems, including epilepsy and high blood pressure. Pete found it very difficult to communicate with his GP, and usually relied on his wife to translate. This meant that not all of Pete’s health problems were addressed or discussed when he went to the doctor, and he often felt excluded from conversations at these appointments. Prior to one of Pete’s GP appointments, I used Talking Mats with Pete to find out how he felt about his health. During our discussions, Pete was able to tell me that he was worried about a number of issues, but he especially wanted to talk to his GP about his ears, as he was having a lot of pain and also had a ringing sensation in his ears which meant that he found it very difficult to concentrate, particularly when watching TV.
Pete took the photo of his completed mat with him to his next GP appointment and his GP used this as a focus for discussions. As a result, Pete was referred to an audiologist for assessment. His GP also spent time discussing Pete’s epilepsy with him and referred him back to the epilepsy specialist nurse who worked with Pete and his wife to improve their understanding and management of it.
Using Talking Mats helped Pete prepare for his GP appointment and also ensured that his GP focused on what was important to him. As a result, time was spent more effectively by all and Pete felt listened to and really participated in his GP consultation.
Use the Talking Mats ‘health’ symbols from the health and well-being resource to help people prepare for appointments with health professionals and manage their health more effectively.
When people have been in hospital for a period of time, for whatever reason, consideration needs to be given to discharge planning. There are often concerns about what a person may manage to do independently when they get home, and this often has an impact on where people are discharged to and what type of support they might need.
The ‘looking after yourself’ symbol sets in the health and well-being resource provide a good starting point for exploring some of these issues. This set is made up of three topic sets:
- Domestic life
- Self-care
- Work/education
I used these when I worked with a woman (Ruby) who had severe receptive and expressive aphasia. She had been discharged from hospital with a care package (carers came in three times a day to help her with personal care, meal time preparation and housework). Ruby had difficulty communicating through speech but was able to use Talking Mats effectively to express her views. I used the ‘domestic life’ symbols to find out how Ruby felt about managing the daily running of the household. Ruby was able to tell me that she felt she could now do more things around the house, such as hoovering and the laundry. She was ‘unsure’ about cooking and shopping, but indicated that these were areas that she wanted to work on.
Using Talking Mats, Ruby was able to tell me that she wanted to try to do more things for herself. We used photographs of the completed mats to discuss these issues in more detail with Ruby’s social worker and her husband. Initially, Ruby’s husband was hesitant about her doing more things around the house, but seeing the mat in front of him meant that he really listened to her views and felt happier about her taking risks and trying things for herself. As a result of our discussions, Ruby’s social worker reviewed her care package. She reduced the daily visits by carers and Ruby was given support from the rehabilitation team to help her work on preparing meals. Her husband arranged for a friend to take her to the supermarket once a week so that she felt more in control of the cooking. Use of Talking Mats meant that Ruby was really involved in setting her rehabilitation goals and ensured that her views were heard when her care package was reviewed.
The ‘looking after yourself’ symbols can be used to include people with communication difficulties in the decision making process. This is particularly important given the current legislative drive to promote self-directed support. Find out more about how to use Talking Mats by signing up for a training course at Talking Mats.
In a previous Blog, Joan talked about the four purposes of communication (Light 1988):
1. Expression of needs and wants
2. Information transfer
3. Social closeness
4. Social etiquette
Social closeness can often be overlooked when we support people with communication difficulties, as there can be a temptation to focus on what some see as the ‘important things’ – helping people to express their needs and wants or to transfer information. Social closeness is the glue which binds us together and helps us to form and maintain relationships. It’s really important that we establish this before we start exploring some of the difficult issues that many of the people we are working with face. In my work with people with severe aphasia, I spend time getting to know what matters to them and finding out what their interests are. This is a crucial part of building a relationship with the person and their family. It also provides a much more concrete starting point for beginning to explore rehabilitation goals, as this example shows:
When working with Jack (a man with severe receptive and expressive aphasia), I started by using Talking Mats to ask him how he felt about leisure activities. This was a great way to get to know Jack as a person and to find out his interests. During our conversation, Jack told me that he enjoyed going out for a drink but hated shopping and bingo – and we all had a laugh as he told me this. Jack also told me that he used to like ten pin bowling. He pointed to his leg to indicate that this was something he could no longer participate in as he was now in a wheelchair. I could see that this was important to Jack, so we talked about possible ways round his physical difficulties. Jack agreed that this was something he could work on with the help of his family and the rehabilitation team.
Given that Jack had severe receptive aphasia, if I had started by using Talking Mats to identify specific problems (using a top scale of ‘managing’ and ‘not managing’) as part of the goal setting process, it is highly likely that Jack would have found this too abstract and difficult to engage in. By using the more concrete topic of leisure (with a top scale of ‘like’/’dislike’), Jack was able to reflect on his life since his stroke and tell me how he felt about his restricted physical abilities. I was also able to build up a picture of him as a person and we had fun at the same time.
When using the Health and well-being resource, think about the person you are working with in relation to the ideas and concepts that they can cope with. Exploring leisure activities is a great way to start as it means you can establish rapport by finding out what matters to them.
Have a look at this Blog to see how other people have used a topic such as leisure to build social closeness.
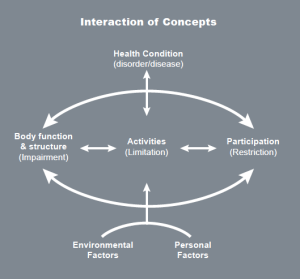
The Health and Well-being resource is based on the WHO International Classification of Functioning, Disability and Health (ICF) which is a framework which covers almost every aspect of daily life and can be applied over different cultures (WHO 2001).
Use of the WHO ICF helps professionals to think holistically about the people they are working with. We have produced four sets of symbols, based on WHO ICF, to help people express their views about different aspects of their lives. These cover 13 topics:
You can use the symbols in different ways, depending on the cognitive abilities of the person you are working with. For example, if you are working with someone who can understand abstract concepts, you could start with the 13 main health and well-being symbols. Your top scale might be ‘managing’ and ‘not managing’. Here is an example of a mat completed by Duncan who had a stroke which affected his ability to communicate through speech:
Using these symbols as a starting point, Duncan could tell us that his main concerns related to worries about his health, expressive communication and work. From here, we did ‘sub mats’ to help Duncan identify the specific areas he wanted to work on/explore.
Here is the mat Duncan completed in relation to his health:
Having done this mat with Duncan, it became clear that he was worried about various aspects of his health, particularly the risk of having another stroke. The wider team were able to give him and his wife information about stroke prevention. Other mats were also completed, exploring expressive communication, work and education and higher level communication (which is included in the ‘learning and thinking’ topic, and covers written communication as well as memory and concentration). Using the Health and Well-being symbols, we were able to work with Duncan to help him identify the main issues that he wanted to work on and then work towards more specific rehabilitation goals. Duncan had copies of all the mats he had completed and found it useful to refer to them over the months. This helped everybody stay on track in relation to his goals and he was also able to track his progress over time.
Have a look at our Health and Well-being resource on our website. It is available both as an original Talking Mat with a physical mat and symbol cards or as a digital version as part of The Talking Mats pro subscription
I like my iPad and I LOVE the new Talking Mats app.
My 89 year old mum lives on her own about 2 hours from where I live and enjoys looking at photos on my iPad Mum has ‘all her marbles’, as the saying goes, and freely expresses her extreme views on current affairs, politics and photographs in Hello magazine! More difficult however, is discussing her failing energy levels and physical strength. She has till now resisted all suggestions of moving house to somewhere with more support.
I knew she would be interested in the Talking Mats app and a demonstration one afternoon flowed naturally into the Domestic topic of the Health and Well Being section. Suddenly we were in the middle of that difficult conversation we’d both been avoiding. Mum fully engaged with the app and changed the position of some items after consideration
The reality is she isn’t managing, she’s struggling. For the first time using the Talking Mats app she confessed to all domestic tasks being difficult even with the bits and pieces of help going in regularly.
The app made that bit easy. Making a decision about the next step will be more difficult.
Rhona Matthews
The final part of my keynote talk at the AAC Conference in Helsinki last month focused on what we mean by communication effectiveness.
It is important to be able to determine the effectiveness / success of an interaction between two people, whether they are politicians, parent and child, husband and wife….. people using AAC systems or people using their own speech.
When I carried out a literature search of peer reviewed journals for my PhD in 2009 I could find no clear definition of communication effectiveness. Some people thought that effectiveness was synonymous with ‘word intelligibility’ or ‘correct syntax’. Others defined effectiveness in terms of the number of words produced on an AAC device. One publication even suggested that effectiveness was demonstrated by someone taking responsibility for charging their AAC device!
The main focus of all the papers I found, which mentioned communication effectiveness, was on needs and wants and only 3 papers cited social closeness as important (click here to read previous blog).
However, some publications did give useful pointers. Light (1988) emphasised that effective communication depends on 2 way interaction and that the partner is a major factor in the success or failure of communicative interactions. Lund (2006) described adequacy, relevance, promptness and communication sharing as key indicators. Ho et al (2005) highlighted satisfaction – partners’ feeling of how well they communicated during the conversation. Locke (1998) stressed that determining the success of any communication is a subjective undertaking as ‘Communication is not a mathematical formula of phonemes, morphemes and syntax, but rather includes casual conversation such as gossip’.
The Talking Mats team has tried to capture what we believe are the essential factors in determining communication effectiveness. We have produced a simple tool – the Effectiveness Framework of Functional Communication (EFFC) which can be used to chart key factors in an interaction on a 5 point scale and give an overall indication of whether the conversation is effective or not.
We have used the EFFC in several of our research projects and show participants how to use it during our training workshops. In Finland I tried it out with the audience of 200 AAC professionals using 3 video examples of different AAC conversations. The resulting scores were amazingly in agreement suggesting that this is a reliable tool.
For a free download please click here EFFC 2014
We would welcome any comments or questions.
In my last blog I wrote about the purposes of human communication and suggested that social closeness is essential for effective communication. Janice Light, in her 1988 model, described social etiquette as the ability to conform to social conventions of politeness and one of the key purposes of communication.
I believe that social etiquette has been overlooked when working with people with communication difficulties. Social etiquette may be seen as ‘the cherry on the cake’ and not really necessary, when getting a basic message across is so difficult for someone with a communication disability. However, the way in which someone greets you when they meet you, how they show interest in what you are saying or how they say goodbye, all effect how you respond to them and can influence your subsequent interactions with them.
Moreover social etiquette can often be done non-verbally – a smile to show you are pleased to see someone, a nod of agreement to show you are following what they say, a handshake or ‘thanks for coming’/’good to talk to you’ when you say goodbye. These are all basic and almost universal communication symbols.
Social etiquette is not just a communication add-on that can be missed out because it’s too much effort. It can be crucial in developing and maintaining relationships.
For those of us who work or live with people with communication difficulties it’s important that we consider the purposes of human communication. As long ago as 1988 Janice Light suggested that there were 4 main purposes and we believe this is still a good model to bear in mind.
(Light, J. (1988) “Interaction involving individuals using augmentative and alternative communication systems: state of the art and future directions”, AAC, 4, 2, 66-82)
She described these purposes as:
1. Expression of needs and want – to regulate the behaviour of another person to get something
2. Information transfer – to convey information from person A to person B
3. Social closeness – to establish and maintain relationships with others
4. Social etiquette – to conform to the social conventions of politeness
We believe that there is a tendency to concentrate too much on 1 and 2 and not enough on 3 and 4. If we dwell on needs and wants, which is very often the focus of communication aids, there is a danger that the person with the communication difficulty will find it hard to establish and/or maintain relationships.
In 1998 John Locke wrote that ‘small talk’ is crucial for the construction and enjoyment of relationships with others and that by revealing thoughts we elicit reactions from others. This is what we regard as social closeness or engagement. ‘Small talk’ or ‘social closeness’ may sound irrelevant but it is one of the most important purposes of human communication.
(Locke, J. L. (1998) “Where did all the gossip go? Casual conversation in the Information Age”, American Speech Language Hearing Association, 40, 3, 26-31)
Talking Mats, which uses attractive and motivating communication symbols, is one way to help people to express their thoughts and achieve ‘social closeness’, whether they are a 4 year old boy with Downs Syndrome or a 95 year old woman with dementia.
Talking Mats is one of the few resources that is versatile enough to be used as a stroke communication resource, for consulting children and young people or to help with communication difficulties and dementia, to name but three.
It allows people to express their thoughts in a visual way which in turn can elicit a response from their communication partner. Moreover, solid research has shown that Talking Mats increases engagement in people with different communication difficulties.
 Online training login
Online training login