We were delighted to receive this excellent poster from Lora Franceschi who used Talking Mats and the Visual CARE Measure to facilitate patient feedback in a rehab team. Lora works with the Speech and Language Therapy Rehab Team at Queen Elizabeth University Hospital in Glasgow.
The team combined the Visual CARE Measure with the Talking Mats technique to fulfil the following aims:
- Obtain the views of patients (and their carers) on how empathic and patient centred the SLT had been during their inpatient rehab stay
- Establish if the Talking Mats activity could facilitate feedback from patients with moderate-severe communication difficulties
- Determine the time and resource implications in obtaining patient feedback using the above method
- Ascertain whether this format could be rolled out across other SLT teams within Greater Glasgow and Clyde
These aims were all fulfilled and they concluded that this approach could be replicated with other teams and used as a means to gain feedback from patients with communication difficulties.
Click here to see the full poster with their results 2016 QEUH VCM and TM. We think this is such an excellent poster that we have printed it out and put it on the wall in the Talking Mats Office.
You can do the same!
To get copies of the full report please contact Lora at Lora.Franceschi@ggc.scot.nhs.uk
We have been exploring how Talking Mats can be used as a tool to support business – both a framework for interviews and appraisals. Because it supports reflection, it is an ideal framework for employers to use with job candidates.
The recruitment process is time consuming for organisations, and any errors at this stage can be costly for teams. When I applied for the post of associate with Talking Mats I wasn’t surprised that the actual interview was engaging and different from any other interview experience.
The first part was for the candidates to teach the interview panel a skill, in 5 minutes. As a speech and language therapist this made a lot of sense to me, as teaching people a skill is more empowering than merely sharing your knowledge.
The second stage of the interview was using a Talking Mat to consider my levels of confidence in relation to aspects of the post.
Having used Talking Mats with children and parents in my clinical work, I wasn’t used to being ‘on the other side of the mat’, and experienced first-hand the positive aspects.
Firstly, it gives the interviewee permission to break eye contact. This immediately takes away the pressure of non-verbal feedback from the panel e.g. if one of the panel is smiling encouragingly, it is tempting to focus on that one person and possibly say too much. The focus being on the cards and the actual mat can reduce anxiety, supporting people to clearly express their views.
Another aspect of Talking Mats is that the person interviewing, hands to the candidate a picture card on one aspect of the topic e.g. knowledge and skills.
The multi sensory aspect i.e. auditory , tactile and visual, supports the candidate to focus on this one concept and share his or her reflection.
The conversation is then built up and captured on an actual mat and the candidate has the opportunity to move the options on the scale as the conversation progresses.
Talking Mats as a communication tool maximises the capacity of individuals to say what matters to them. How many people leave an interview feeling they didn’t say what they wanted to?
P.S. I got the job!
We are very grateful to Lauren Pettit and her colleagues from Pretoria, South Africa for sending us their published paper on a recent research project which used Talking Mats as a research method.
The study’s aim was to describe and compare the views of adults with aphasia, their significant others and their speech and language pathologists regarding the importance of nine life areas for the rehabilitation of adults with aphasia.
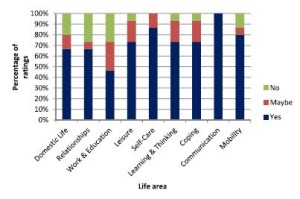
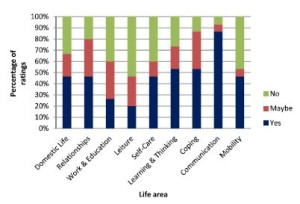
They used Talking Mats to support 15 adults with expressive aphasia to rate 9 life areas in terms of importance to them. The 9 life areas they included were Domestic Life, Relationships, Work and Education, Leisure, Self-care, Learning and Thinking, Coping, Communication and Mobility. These are taken from the World Health Organisation International Classification of Functioning Disability and Health (WHO-ICF). The researchers also obtained the ratings of 15 significant others and the 15 speech and language pathologists treating them.
They found that most life areas were rated as important to work on in rehabilitation by most participants. However, there were some discrepancies between the views of the adults with aphasia and the other 2 groups in the study and significant discrepancies were noted for 3 of the 9 life areas.
The graphs below show the comparisons of the 3 groups of participants. Click on graphs to enlarge
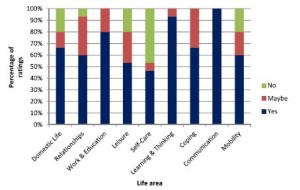
The researchers suggest that ‘These life areas can provide the ‘common language’ for team members to engage in dialogue and identify problem areas related to the daily life functioning of people with expressive aphasia. By simplifying some of the labels of the activities and participation dimensions of the WHO-ICF and pairing these labels with pictures and the interactive Talking Mats interview procedure, adults with expressive aphasia (who often have difficulty participating in the selection of rehabilitation priorities) were able to express their own views. This may be a first step in assisting the adult with aphasia to advocate for themselves and to exercise their right to identify the activities and participation opportunities which they would like to access, and to set rehabilitation priorities based on their choice. While the overlap in priorities among the three groups as found in this study is encouraging, the presence of some significant differences underlines the importance of the voice of adults with aphasia themselves. This ensures truly client-centred rehabilitation that underscores the principles of human rights and a focus on competence rather than deficits’.
To link to the full article: http://dx.doi.org/10.1080/10749357.2016.1207148aphasia
Please contact info@talkingmats if you would like to discuss using Talking Mats in research
Castle Hill High School has seen the benefits of using Talking Mats to let pupils have their say and be involved in planning outcomes. Jenna McCammon, Speech and Language Therapist & Rebecca Highton, Speech and Language Therapy Assistant, Stockport NHS Foundation Trust explain how they are using Talking Mats at Castle Hill High School.
Talking Mats has been beneficial in supporting young people with communication difficulties in school.
A Talking Mats approach has been used to support a pupil who presents with selective mutism. He started refusing to engage in lessons and activities, so school wanted to find out what he enjoys doing and how best to support him. Talking Mats allowed the speech and language therapy team to find out about his likes and dislikes at school, along with the reasons why he was refusing to engage in certain lessons. The sessions allowed the speech and language therapy assistant to build rapport with the pupil through finding out what he enjoys both in and outside of school, and the pupil communicated verbally during one of the sessions for the first time since his change in behaviour. The speech and language therapy assistant took pictures of the finished piece of work and asked permission from the pupil to share this with school staff. The speech and language therapy assistant was able to feed back the outcomes with staff and with other professionals during TAC meetings. Staff and other professionals would then request if the speech and language therapy assistant could obtain more information from the pupil, when needed, using Talking Mats.
Safeguarding – A possible safeguarding issue was suggested by a pupil during a therapy. The pupil has significant communication difficulties and so the information she was able to provide was very limited. The safeguarding officer in school requested if the speech and language therapy team could try to find out more. This was done us using Talking Mats, which allowed the pupil to share more information about the issue which was then shared with the safeguarding officer.
Motivational Interviewing is a tool used by the speech and language therapy team, both when assessing a new referral and when completing a review assessment in order to set new therapy targets. It is an opportunity for the young person to express their opinion, and can also be used to determine how much insight they have regarding their communication abilities. This is usually done verbally using a 10-point scale, however Talking Mats has been used by the speech and language therapist when assessing pupils with limited verbal ability. This allows these pupils to voice their views and have a say in their therapy planning. The findings from the Talking Mats motivational interviews then contribute to writing EHCP Reports for the pupil and are used to inform the decision-making process regarding their therapy goals.
Thanks to Jemma and Rebecca for sending these great examples. Change happens when we give young people a listening space.
This blog summarises a project we have completed providing Talking Mats training for families living with dementia. A key aspect of the work done by Talking Mats is to find ways to improve communication for families living with long term conditions. In particular dementia is a long term condition where deterioration in communication will eventually affect everyone. This makes it increasingly difficult to ensure that the person with dementia continues to be involved in decisions about their life.
We have completed a project funded by Health and Social Care ALLIANCE Scotland. Training in the use of Talking Mats was given to families living with dementia and staff who worked with these families. The Alliance Family Training final report highlights how this training helped people with dementia to communicate their views and be more involved in making decisions about their lives.
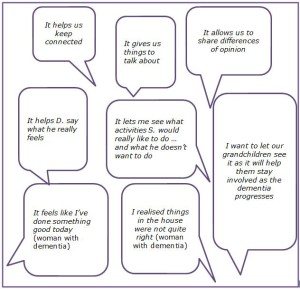
Families identified issues relating to self-management that they had not previously been aware of and new insights emerged as the following comments illustrate.(click on box to enlarge)
For some family members an important outcome was that Talking Mats helped them see that their spouse was satisfied with many aspects of his/her life. They found this very reassuring as many assumed that the person with dementia was frustrated and discontented.
The following is an example of how using Talking Mats helped with self-management.
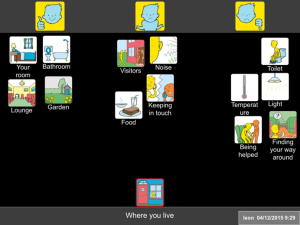
When using Talking Mats on the topic of Where you live, G explained that he found it difficult to find his way to the toilet in the night. As a result his wife bought special senior night lights to help him which solved their problem. As a result, night times improved for both of them.
For further examples and information read the full report here Alliance Family Training final report and for further information about Talking Mats Family training please contact info@talkingmats.com
Thanks to Agnes Turnpenny for her guest blog on her research on views of people moving form institutional care in Hungary.
There are approximately 15 thousand adults and children with learning disabilities living in large institutions in Hungary. The average size of these facilities is over 100 places, and living conditions as well as the quality of care are often very poor. The Hungarian Government adopted a strategy in 2010 to close and replace these institutions with smaller scale housing in the community. Between 2012 and 2016 six institutions closed and more than 600 people moved to new accommodation. The Mental Health Initiative of the Open Society Institute and the Hungarian Civil Liberties Union commissioned a study to analyse the experiences of the deinstitutionalisation process and as part of this research we carried out some interviews to explore the views of people moving out of the institutions.
The participants – five men and four women – came from one institution in the North East of Hungary, they all had mild learning disability and some had additional mental health issues. Originally the study intended to explore the experience of moving out but due to delays in the project this was not possible. Instead, we decided to examine the expectations of moving from an institution to a smaller home that allows more independence and personalised support. Although only one of the participants had communication difficulties – thus conventional interview methods could have been utilised – I decided to use Talking Mats in order to help participants to contrast their current situation with expectations about the future.
I selected the ‘Where you live’ topic from the Social Care package with some additional images from the ‘Leisure and Environment’ and ‘Relationship’ topics. (The English labels were covered over with a Hungarian translation as most of the participants could read). The question I asked was “How do you feel about these aspects in the institution?” and “What do you think they will be like in the new home?”. (I forgot to take a mat with us, therefore we had to lay out cards on the table.)
It emerged – unsurprisingly – from the interviews that most participants anticipated the improvement of their living conditions from the move, especially better facilities (mainly bathroom and kitchen). Some also expected other positive changes, particularly less conflict with other residents, less noise and better safety –commenting on the prevalence of theft in the institution. There were also many uncertainties; people said they were unsure about how they would get on with their new housemates, how the new support arrangements with staff would work, whether the neighbours will be welcoming etc. The photos illustrate some these issues.
Overall, Talking Mats proved to be a very useful tool in interviewing participants, who really engaged with the method. The images and the completed mats encouraged further comments and explanations on issues that participants considered important with minimum prompting. The drawings were easily recognised and appropriate in the Hungarian context without any adaptations other than the labels. Finally, I felt that the use of Talking Mats in this particular situation helped to overcome some of the power imbalance between the researcher and the participants by giving them more control when handing over the images.
We are really grateful to Agnes Turnpenny from The Tizard Centre University of Kent for sharing her experience . We really value our European work and European connections.
Thanks to Laura Holmes for telling us more about the innovative work in Stockport.
As part of an ongoing project, we at NHS Stockport Children’s Speech and Language Therapy Service are introducing the Talking Mats approach to support the children we work with to contribute to their own EHC Planning, enabling them to make their voices heard.
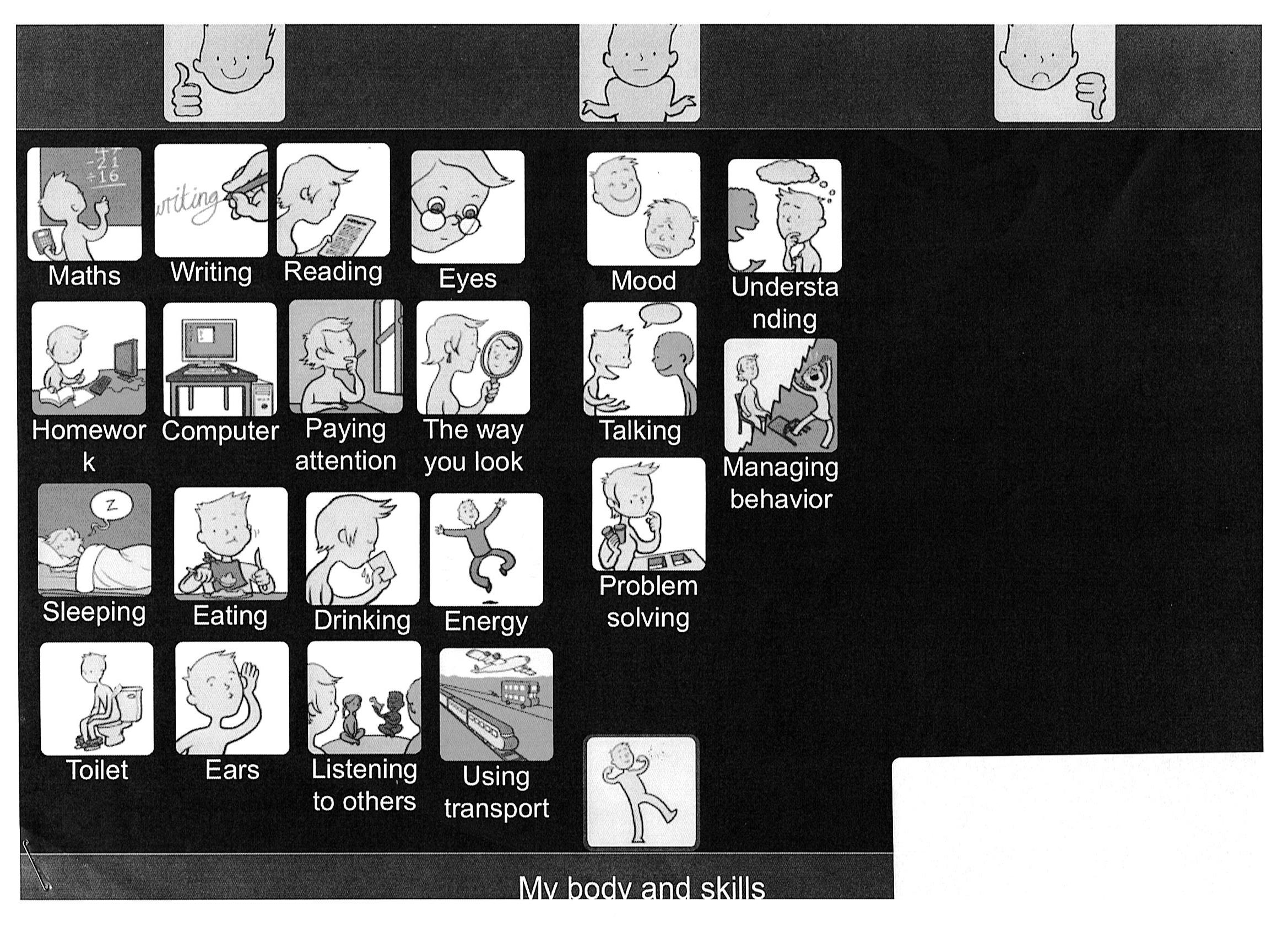
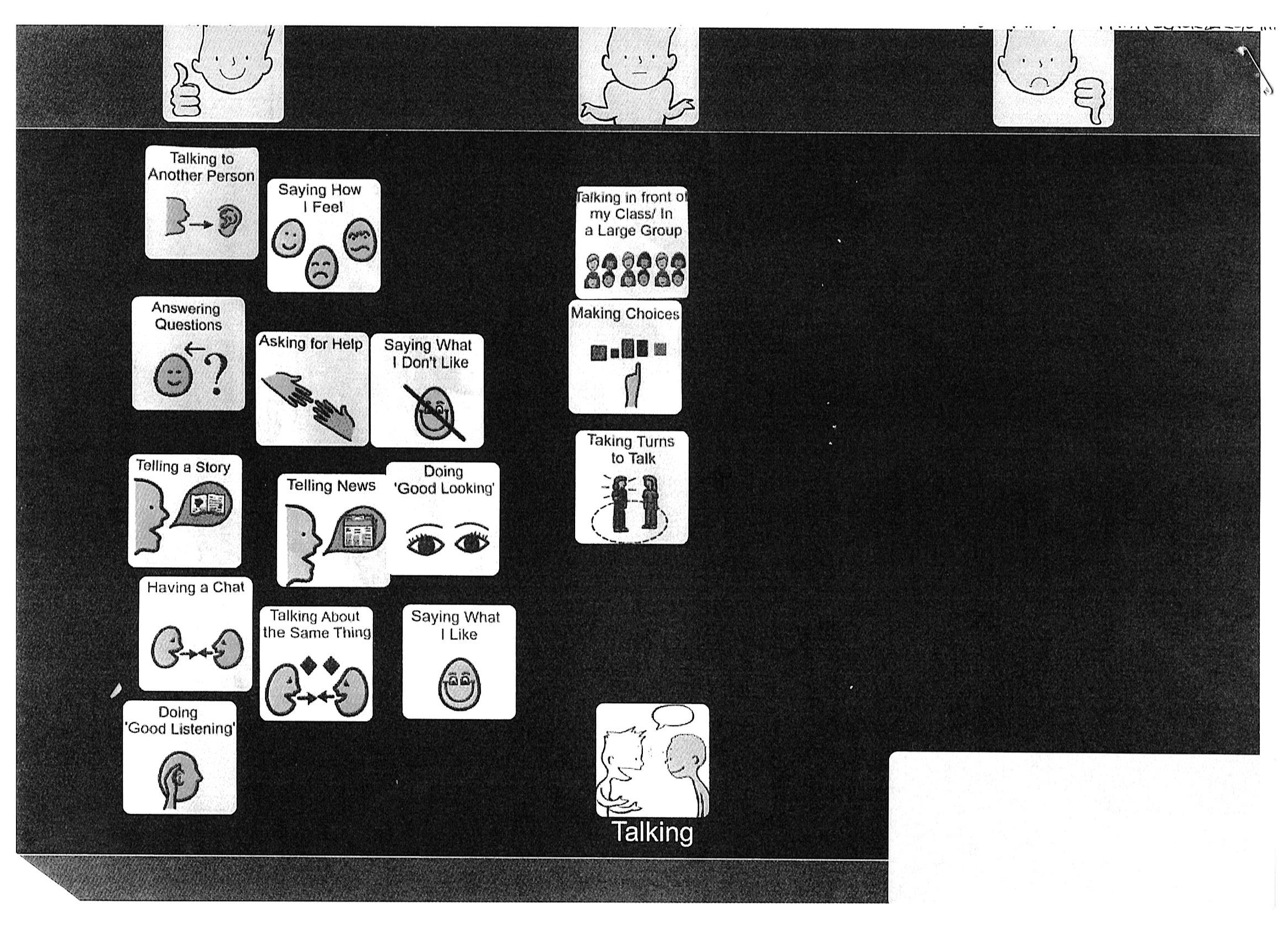
For example, I have used the ‘Consulting Children and Young People – My Body and Skills’ (Primary) digital resource to help identify and plan target areas for an 6 year old child with a diagnosis of Autism. I selected a top scale of ‘happy/unsure/not happy’ and chose a variety of options symbols from the resource. The child (R) was then able to drag and drop each option symbol to the area she felt it belonged in, producing the following talking mat:
Whilst completing the mat the child volunteered further information about particular options – in general I find I get to know the children I work with much quicker using this approach!
Once complete, we agreed that we would sub-mat the option ‘talking’ (which had been placed under ‘unsure’) and explore that option as a topic in our next therapy session.
I then thought about all the possible options I wanted to explore in this submat, and created symbols using Boardmaker. I was able to add these symbols as options for the digital mat by taking photos using my Ipad and selecting them from my camera roll.
R completed the submat as follows:
The mat enabled R to pinpoint the areas of talking she feels unsure about – i.e. ‘talking in front of my class/ in a large group’; ‘making choices’; ‘taking turns to talk’. I was then able to include this information in my review report, attaching the pictures of the mats as evidence of consultation. My review report included details of specific targets and recommendations to support R to work on the areas she had identified, which are designed to be incorporated into her EHC Plan.
We know from our own network that many practitioners are looking for training and tools to help implement the SEND reforms. Talking Mats are running a free seminar in Stockport to let practitioners see how Talking Mats can be used. The morning session is FULL but we have added an afternoon session. Book your place now as it is first come first served and places are filling up fast. Free Stockport afternoon seminar
Talking Mats considers both health and social aspects when it is used to include people in their care planning. Lots of interesting comments are made by course participants on the forum in our online training course. Annemarie, who works as an agency carer visiting clients in their own homes posted her thoughts about the social model of disability
Remembering the person behind the condition
In my experience, society is fixated on the medical model, the ‘what’s wrong’ approach. Whilst the medical model is clearly a valuable and required tool, it often leads to labels that individuals are then lumbered with, such as, ‘she has dementia’, ‘she is visually impaired’, ‘he’s deaf’ or has a ‘leaning disability’. Taking this approach overlooks the person behind the ‘condition’ and so can restrict inclusion. One example could be an individual with dementia being unable to make everyday choices about seemingly mundane issues such as what to wear that day. Using a medical model, a carer may be aware of the clients difficulties and make choices for them, whereas using the social model approach enables the carer to see beyond the condition and fully include the client, allowing them to be part of the decision making process for themselves. A second example could be a person with a communication disorder such as Asperger’s Syndrome. Access to work could be severely restricted using a medical model as the pragmatic manifestation of this condition may well exclude a person from seeking certain types of employment. Promoting the use of a social model would ensure work colleagues understood the possible limitations of the condition and ensure adequate support networks were in place. The social model attempts to embrace a person’s difference and raises awareness within society of individual needs that will facilitate inclusion into all aspects of life.
The WHO ICF -World Health Organisation International Classification Framework of Functioning, Disability and Health (2001, 2007b) aims to merge the medical and social model, encouraging professionals to think not only of the persons health condition and resulting impairment, but the impact this has on the persons participation and activities. It captures the full complexity of people’s lives, including environmental and social factors and can be applied over different cultures
The Talking Mats Health and Well- being resource is based on the WHO ICF and supports a person to reflect and express their view on various aspects of their lives. Using the Health and Well being resource supports workers to remember the person behind the condition.
Thanks to Laura Holmes for telling us about the innovative work in Stockport.
The new SEND reforms in England, as described in the SEND Code of Practice: 0-25 years (2014), have highlighted the need for health, education and social care professionals to involve children and young people in decision-making processes, in particular, during the assessment, production and review of Education, Health and Care (EHC) Plans.
In NHS Stockport Speech and Language Therapy Special Needs Service, we have recognised this need and are in the process of introducing the Talking Mats approach to enable the children we work with to share their views and opinions – i.e. to hear the ‘Voice of the Child’. We also obtain the views of parents/carers and school staff through use of questionnaires. These views and opinions are then incorporated into a child’s Individual Therapy Plan and consequently their EHC Plan.
Children with Speech, Language and Communication Needs (SLCN) can often struggle to express their views and opinions. We have found that Talking Mats is a highly effective way of gaining the views of the children and young people we work with, whether they are verbal or non-verbal. Talking Mats enables them to become involved in their own therapy planning and interventions, which in turn feeds into the EHCP process.
In addition, the Talking Mats approach links well with the use of Therapy Outcome Measures (TOMS), particularly in relation to the evaluation of the general activity, participation and well-being of a child/young person. TOMS is the outcome measurement tool recommended by the Royal College of Speech and Language Therapists (RCSLT).
In my next blog, I will provide an example of how Talking Mats has helped the children we work with to participate in the EHC plan process.
We know from our own network that many practitioners are looking for training and tools to help implement the SEND reforms. Talking Mats are running a free seminar in Stockport to let practitioners see how Talking Mats can be used. Book your place now as it is first come first served. Free seminar Stockport
Engaging with people who have difficulty communicating can take time and may result in misunderstandings which can cost a lot in terms of time and cost and emotion for all involved. Research and anecdotal evidence have both shown that using Talking Mats is efficient and cost effective in that staff or carers can get better quantity and quality of communication with the people they work in a shorter time with than with usual methods of communication. The average time for someone trained in Talking Mats to have a Talking Mats conversation is 15 minutes, although some people may choose to talk for longer.
In addition, staff often rely on relatives to gather information about a person’s needs and preferences. The process of gathering that information can be protracted owing to availability of family members and, because it is second-hand, is liable to misinterpretations. This in turn can lead to frustrations which can damage relationships, result in poor care and cost time.
At a practical level, the feedback from staff has been that the wipe clean, ready-made Talking Mats symbol sets give immediate access to a practical communication tool. Staff compared this favourably with the time taken to source images on-line, print them out, cut them up and develop them to a standard that is infection control compliant.
The Talking Mats team have invested their time and skills over several years to develop topics which are based on sound research. For example the Health and Well-being Resources is based on the World Health Organisation ICF, the Children and People’s Resource is based both on WHO-ICFCY and GIRFEC. The Eating and Drinking Resource has been co-produced with people with eating and drinking difficulties and a range of different professionals. The Talking Mats symbols have been carefully designed to represent both concrete and abstract topics
In addition sending staff on a Talking Mats training course results in a work force which is effectively trained in communicating with a wide range of people as well as having a bespoke communication tool. Using Talking Mats is efficient for organisations both in terms of time and costs.
 Online training login
Online training login