Covid 19 Experiences – Using Talking Mats in a Secure Hospital Setting
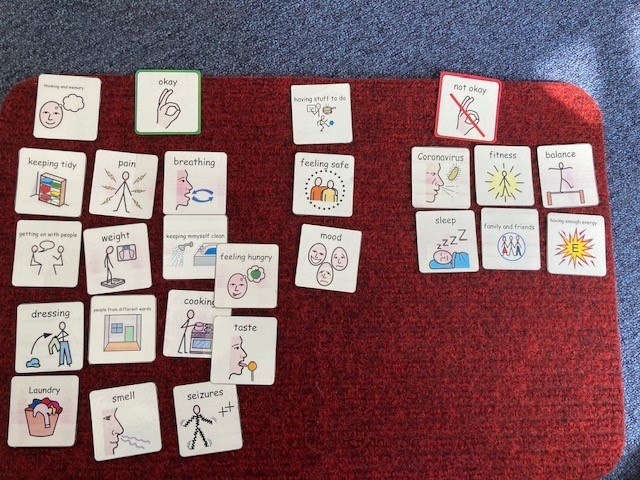
As a group of Allied Health Professionals (AHPs) working in a secure hospital we recently embarked on a mini project using Talking Mats to check in with our service users with learning disabilities during Covid-19. We collated the evidence from our respective professional bodies (Royal College of Occupational Therapy, Royal College of Speech and Language Therapy, Chartered Society of Physiotherapists and British Dietetic Association) in terms of changes that people might experience if they’d had Covid-19 and produced a talking mat around these.
It quickly dawned on us that we might be on to something here, and that creating an opportunity to ‘check in’ more broadly with our service users would serve a useful purpose, so we added some additional categories around changes to routine, psychological wellbeing and feeling safe.
This was my colleagues’ first experience of using talking mats, and their faces when I turned up clutching my 99p actual doormat were a picture! I introduced them to the theory behind the mat and its presentation and harped on about the benefits in terms of attention, comprehension, non-threatening interaction, initiation and structuring narrative; they nodded supportively.
We set off across our learning disability wards in multi-disciplinary pairs and all but a few of the service users agreed to have a chat with us. My colleagues commented that they were pleasantly surprised by the engagement and the amount and novelty of the information gained; we identified things that the service users hadn’t told anyone because they hadn’t been asked that question!
In talking to others we were asked why weren’t rolling this out in a partner secure hospital for people with mental health conditions? ‘no reason really, we just haven’t got there yet’ we answered. Then came the…. but we can just do it like a questionnaire with them. This question wasn’t, and in my experience isn’t ever ill meant. It comes from a place of naivety in relation to the presence of communication difficulties in people with mental health conditions and because of that, lack of exposure to different professional groups such as Speech and Language Therapy and the skills and approaches we have to offer. Skills in gaining and holding someone’s attention. Skills in decreasing pressure in communication situations. Skills in enabling time, space and ways in which people can initiate their thoughts.
The Multi-Disciplinary Team (MDT) working around the project has enabled me to show others how talking mats can support their practice. It has enabled them to see how a very simple and non-threatening visual tool can open up conversations and lead to information that the service users hadn’t shared before, in a way that a face to face conversation doesn’t.
Thanks to Jo Brackley, Clinical Lead, Speech and Language Therapy Secure Services at Cumbria, Northumberland Tyne and Wear NHS Foundation Trust for this inspiring blog – which demonstrates when we shift the way we listen and gather information from patients we get a different result and improve the quality of information and communication . If you or your team want to consider Talking Mats training then we can provide this for organisations . At the moment we can take a cohort through our online course together and then arrange a zoom call to discuss application to your work setting – email info@talkingmats.com for more information.
 Online training login
Online training login