The first week of January is barely over and we are about to tantalise you with 3 new Advanced online training sessions.
This format has proved very effective to introduce and support the use of our new Advanced Resources for those already trained in Talking Mats. Between February and June we will hold Advanced online training for;
- Sexual Health and Relationships
- Thinking Ahead * new edition for 2025
- Capacity – a resource to enable supported decision making.

What does the Advanced training look like?
- It is delivered live via Teams and facilitated by expert practitioners in the field
- The numbers are limited to allow interactive activities and discussion.
- It aims to improve skills and application for practice.
- It lasts for 3hrs (comfort breaks are included!)
What does it include?
- Why this resource is needed.
- How to use the Resource in practice.
- The opportunity to reflect and consider the impact of using this resource.
- Questions and feedback.
Cost?
£95 including resource
February to June 2025. .
- 5th February 1.00pm – 3.30pm – Sexual Health and Relationships SOLD OUT! New dates coming soon
- 19th March 9.30am – 12.30pm – Thinking Ahead 2025 edition.
- 24th April 9.30am – 12.30pm – Capacity, enabling supported decision making. (date to be confirmed)
There are 30 places available for each event on sale in the shop on our website.
You will only have access to the Advanced training if you have completed the Foundation Training and have an account on our website. If you are unsure or cannot see the Advanced training in the shop please contact info@talkingmats.com
Want to come on the Advanced Training but not yet Foundation Trained? Find out how to make 2025 the year you become a Talking Mats practitioner.
Our thanks for this guest blog go to Meredith Smith, Paediatric Physiotherapist and Lecturer in Physiotherapy in the School of Allied Health Science and Practice at the University of Adelaide. In this blog, Meredith talks about the development of a Talking Mats resource to facilitate self-reporting in pain assessments for children and young people with cerebral palsy.
Our research team has been working on modifying pain assessment tools so they are more appropriate, relevant and accessible to children and young people with cerebral palsy (CP). People with CP have varying functional, communication and cognitive abilities, which makes existing assessment tools (often pen and paper questionnaires) difficult to use across the spectrum of ability. As a result, children and young people with CP often don’t have the opportunity to self-report how pain is impacting their function.
We are based in Australia and our team is made up of physiotherapists, an occupational therapist, a medical practitioner, researchers and people with lived experience of CP. One of the first things we did as part of this project was to ask people with lived experience of CP and clinicians what we could do to make two specific pain assessment tools more accessible and relevant to people with CP and different abilities. One of the clinicians (a speech pathologist), suggested we consider a Talking Mat alternative for each of the assessment tools. These two assessments focused on two concepts – 1) how pain interferes with function and 2) pain-related fear. We were keen to focus on these assessments as this would help us to not only open up a conversation about pain with children and young people with CP, but would also provide us with a way of identifying children who might benefit from particular pain interventions, and allow us to monitor the effectiveness of these interventions.
Prior to this suggestion I had heard of Talking Mats but never used it. Our research team underwent Talking Mats foundation training which was excellent, and we were all really impressed with the concept and its application in varying contexts. We had initially thought that we might need a Talking Mat to get feedback from children on the assessment tools, but we all agreed that converting the pain assessment itself into a Talking Mat would make the most sense for now.
Working with the Talking Mats team was a fantastic experience. We all really appreciated the expertise of the consultants in considering how we worded some of the assessment tool items. The symbols created were also excellent, and when we tested them with children and young people with CP they were simple and easy to understand.
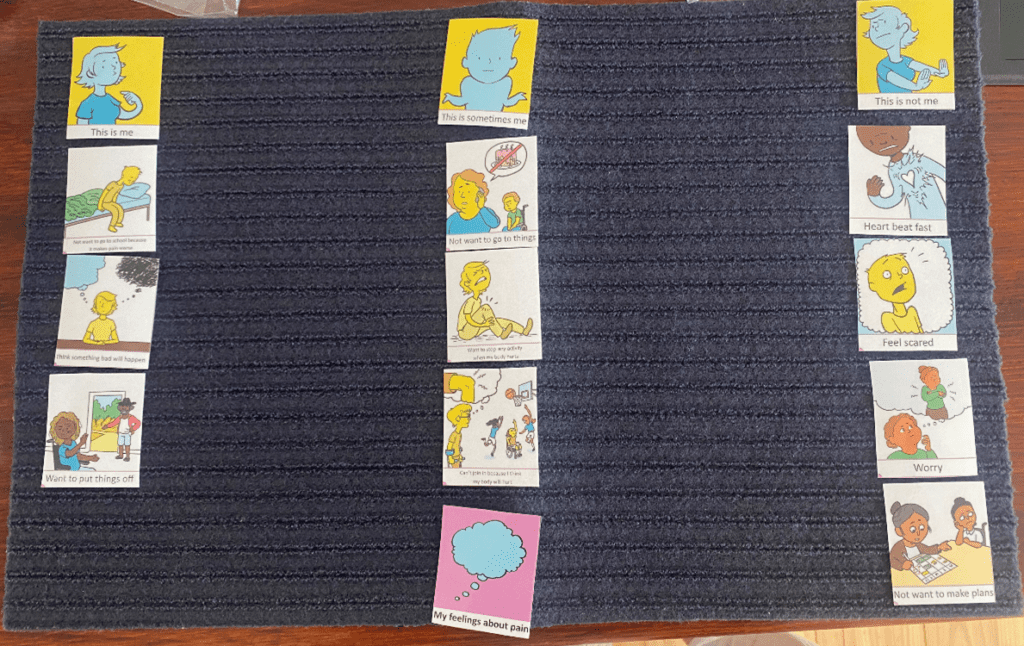
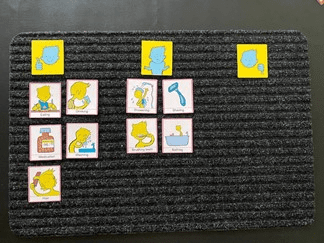
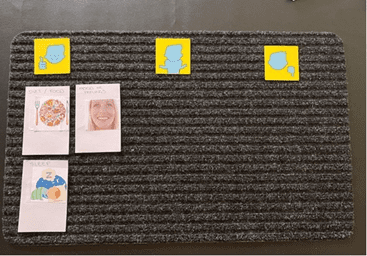
Here is an example of a Talking Mat discussing pain interference with function. The lead in phrase is ‘how much does pain get in the way of……’. This Talking Mat was easily understood by most children with CP, even those with moderate cognitive impairment and complex communication needs.

The second Talking Mat looked at pain related fear, with the lead in phrase ‘pain makes me……’. This was a more challenging and abstract concept, but was much easier to explore using the mat than on a standard pen and paper questionnaire. The Talking Mat versions can be interpreted as a 5-point response scale (the three response options and then two in-between sections), allowing us to still total an overall score for the assessment.
The feedback from children, young people and their families has been very positive. Families of children with cognitive impairment or complex communication needs have shared with us that previously it was assumed that their child could not self-report pain, and often they were asked to proxy-report on their behalf. Parents have told us how difficult it is to proxy-report on personal concepts such as pain-related fear, and that they couldn’t possibly know for certain how pain was making their child feel.
We are in the process of continuing to test the Talking Mats resource and look forward to making the it more widely available in the future.
Keep an eye on our website for more information about the Pain Assessment Resource as this project progresses.
If you are interested in completing Talking Mats Foundation Training, you can find out more here.
We are delighted to share this latest guest blog from Debbie Mole, Clinical Nurse Consultant in Mental Health and Intellectual Disability for DHM Mental Health Care in Melbourne, Australia. This is a great example of the positive impact Talking Mats can have for people who have experienced trauma.
Throughout my 35 year career I have always had a big interest in finding ways to help clients express themselves. My passion is around trauma and working in creative ways to help bring some closure and recovery for the person.
This desire grew when I met a woman who had multiple disabilities. She was blind, deaf, and non-verbal. She was sensitive to touch and had very few ways to express herself. She needed to be admitted to hospital as she was unwell, we had no way to explain to her what was happening. At the time I was working in a new specialised mental health and disability team. This humbling experience of working with her pathed a way for me to find ways to help people communicate and understand.
Working in mental health I am acutely aware of risks and that so many people who struggle to verbalise thoughts, feelings, and past issues. I was always concerned that because a person could not verbalise their thoughts, feelings, and intentions that so much information and potential risks were being missed.
I heard about Talking Mats training in Australia and booked myself on the course. This inspired me and has helped me support clients to find a voice and solutions to issues.
My client was a 30-year man with Down Syndrome, he also has ASD and over the last five years had lost his ability to speak. When I met him, he had poor eye contact and appeared to be locked into his world. It was evident he was also suffering from psychosis as he was responding to auditory and possibly visual hallucinations. He could use some sign language to communicate. He had chronic OCD and anxiety and sleep was a major issue.
I did a Talking Mat exercise and checked his understanding of “like”, “don’t like” and “not sure”. I did a simple exercise to start using the images for his family and carers. There was no real form and the cards appeared to become a collection of images that did not hold any clues.
I decided to use to the personal care cards, this was very different. Showering, bathing, and going to the toilet were placed in the negative area. There was also a change of behaviour and some vocalisation of words that made no sense. Talking to his team and mother, there was a restive quality to his behaviour – he wanted to avoid this area.
I did further assessments and his mom believed that in the past when he was young, he may have experienced some bullying, she also feared that he had suffered some form of abuse. Through the assessment it also transpired that my client was one of five children, all had a significant mental health issue. I organised a specialist to see him and he was diagnosed with Schizophrenia. He was treated with antipsychotic medication.
As the psychosis was being treated his team became aware that my client was starting to talk, it was not clear, but the content had a theme. Tragically themes, names and places started to be spoken about. When he spoke about these events his OCD behaviours of arranging his items on the floor became more chaotic. He spoke of trauma from other boys that took place in bathrooms.
I worked with the client and introduced some basic trauma work, simply allowing him to say what he wanted to and then helping him to realise that he was safe and that was the past. His team did the same. We offered choice about showering, bathing and looked at ways it could be fun or a nice activity to follow. The idea was to change his thinking around baths and showers and for him to realise he was safe and free from threat. We used the talking mats to build upon the things he liked.
I repeated the Talking Mats exercises three, six, nine and twelve months after treatment.
After the psychosis was treated, we became aware that the client looked sad and flat. There was a loss of interest in social activities and there was a lot of talk about the past. We assessed that he was depressed and that it was possible that his recall about the past was becoming clearer. He was commenced on an antidepressant and monitored intensely. We also needed to address the sleep issues. His OCD had led to his bed to being covered in items. We later realised that this helped reduce his anxiety when he was heightened.
My client has regained some speech, I believe he was locked in a world of trauma and psychosis. Now he mentions the names of some of the people who have hurt him. His team reassure him that he is safe, that was the past, and he is ok. He seeks physical attention when he distressed, and he is acknowledged and reassured. We cannot offer typical trauma therapy to him, but just helping him unlock his thoughts, knowing that what was happened was wrong and being heard is healing.
I have since developed my own set of cards, based on the Mental State Examination. I use these to expand on issues and focus on problem areas. These cards talk about perceptual issues, thought problems, beliefs and risks, all areas that are typically private and too often unexplored. The cards have images on them, so clients who struggle to verbalise can use the same system as the talking mats.
Talking Mats allowed me and his team to see things from a different angle. There were many hypotheses used to gain an understanding of his behaviour. This led to effective treatment and partial recovery.
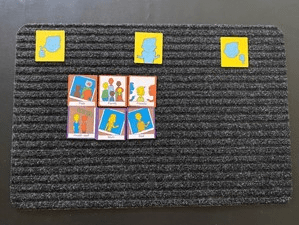
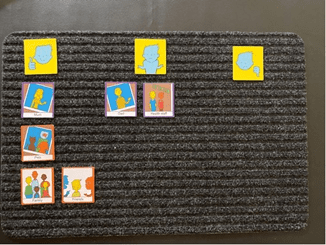
Picture 1 at the assessment stage, images of the clients family were made into an orderly collection with no clear indication of how he felt towards the images:
Picture 2 was also at assessment, showing a clear ability to like, not like and feel unsure about aspects of self care.
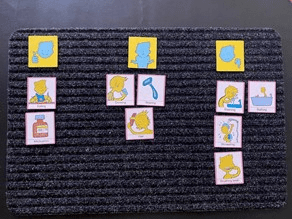
Picture 3 was during treatment for Psychosis and therapy – some changes were being noted with his self care and allowing his team to help him:
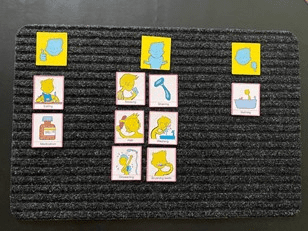
Picture 4 was towards the end of treatment and intensive therapy. Some aspects of bathing remained unsure, but his behaviour indicated that he was more comfortable with activities around bathing.
Picture 5 was a repeat of the family cards after treatment:
Picture 6 are the cards I have created based on the Mental State Examination – this was six months into therapy and medication. He expressed issues around his mood, thoughts and sleep – these needed more explaining. With the mood pictures, I offered my client different images for mood and he picked the ones that reflected what he was feeling. My mood collection has happy, angry, scared and sad in them as I tend to quote these 4 basic raw emotions daily in my work:
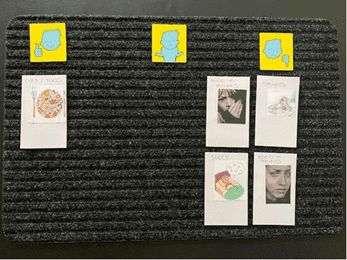
Picture 7 was at the end of treatment the same cards were used with a very different result. As for the previous mat, for the mood pictures, I offered my client different images for mood and he picked the ones that reflected what he was feeling:
Many thanks to Debbie Mole for sharing this powerful example. If you would like to read more about Talking Mats use in Mental Health, take a look at top 10 blogs here: https://www.talkingmats.com/top_10_mental_health/
If you are feeling inspired and have not yet accessed our Talking Mats Foundation Training Course, find out more here:
By Nyaka Mwanza
Multiple sclerosis (MS) can result in a variety of communication difficulties. While broaching uncomfortable topics, such as multiple sclerosis life expectancy, can pose its own challenges, MS can also physically disrupt some people’s ability to communicate as effectively as they once did.
That’s because MS is an immune-mediated condition that damages and destroys neurons in the central nervous system (CNS). Known as demyelination, this destruction of nerve cells causes lesions in the spinal cord, optic nerves, and brain. MS lesions in certain areas of the CNS can sometimes result in difficulties with speech and comprehension. However, there are ways of overcoming these difficulties so that a person may communicate better.
How MS Disrupts Information Exchange
Communication issues in people with MS usually arise due to damage in areas of the CNS that are responsible for cognitive and motor function.
Cognitive Impairment
Cognition refers to our ability to think, read, learn, remember, reason, and concentrate. Cognitive processes also comprise language, planning ahead, imagination, and perception.
Approximately 70 percent of people with MS experience impairments in these cognitive functions. Cognitive difficulties such as slower processing speeds and worsened memory can impede a person’s ability to process spoken or written language. Cognitive impairment in a person with MS may also look like difficulty finding the right words for things when speaking, difficulties spelling words correctly, or switching words incorrectly when speaking.
Language and Speech Difficulties
Speech and language involve several cognitive functions, but speech also involves intact motor function, especially the coordination of the muscles in the lips, tongue, vocal cords, and diaphragm. However, MS can disrupt the brain’s ability to communicate properly with various muscles in the body, sometimes interfering with the ability to produce appropriate speech.
Dysphonia is a voice disorder due to weakened diaphragm functioning. The diaphragm helps with breathing and volume control. Dysphonia can result in very quiet or loud speech. A person with dysphonia may also find that they run out of air while talking. Dysphonia can also cause a raspy voice.
Dysarthria is a motor speech disorder commonly caused by the weakening of muscles used for speech, swallowing, and breathing. Between 40 and 50 percent of people with MS experience passing or permanent dysarthrias, which may result in slurring, monotone, and disruptions to speech patterns with abnormally long pauses between syllables or words. Issues like these can make holding a conversation difficult or uncomfortable.
Bridging the Communication Gap
A speech or language pathologist is a specialized healthcare provider who can evaluate and help treat voice and speech disorders. Depending on the severity of a person’s MS, some speech therapy will focus on compensating for dysfunctions in cognition and speech and enabling people with MS to find alternative means of communication. Other therapy for more mild speech difficulties may focus on developing strategies to control breathing, strengthen the vocal cords, or even simplify speech to make it easier to get through. People with MS may find it’s easier to hold a conversation when they’re not competing with other noises or distractions. Tools that aid with cognitive dysfunction, such as Talking Mats, can help loved ones concentrate on common topics to help make discussion easier. Here is an example of how Talking Mats helped some with multiple sclerosis to set their goals https://www.talkingmats.com/getting-root-problem/
References
- MS Prognosis: Multiple Sclerosis Life Expectancy
- https://my-ms.org/anatomy_nervous_system.htm
- https://my-ms.org/mb_cognitive.htm
- Speech and Swallowing
- Multiple Sclerosis and Communication Difficulties – East Sussex Healthcare NHS Trust
About the Author
Nyaka Mwanza is a freelance writer for MyHealthTeams. She completed a B.A. in Communications: Visual Media from American University and undertook post-baccalaureate studies in Health/Behavioural Communications and Marketing at Johns Hopkins University. Nyaka is a Zambian-born, E.U. citizen who was raised in sub-Saharan Africa and Jacksonville, N.C. However, she has called Washington, D.C., home for most of her life. For much of her career, Nyaka has worked with large global health non-profits focused on improving health outcomes for women and children. Nyaka believes words hold immense power, and her job is to meet the reader where they are, when they’re there.
It’s always great to see pictures of Talking Mats on social media. The stories behind them, and the positive changes that can result for people keeps us motivated to share this powerful tool.
It is apparent however that not all pictures that are called Talking Mats are actually Talking Mats! For example,
TOP SCALES If the top scale is Yes / No Or a tick /cross
It is apparent from these mats that the questions are likely to be closed, and don’t provide a scale for reflection. Closed questions can be leading and suggestive of a set answer the listener is seeking. e.g ‘Did you enjoy your lunch?’ v. ‘How was your lunch?’
A yes/no, or a tick and cross at the top are occasionally used with topics which appear to test understanding of rules, e.g acceptable and unacceptable behaviour in a classroom. In that instance the listener facilitating the mat keeps the control and the power imbalance that exists in conversations for people with communication difficulties isn’t reduced.
The top scale used with each topic is key to the mat working. A Talking Mat could find out what the person thinks about the rules, and which ones they feel are good -not good or help -not help. Our Foundation training includes how to match the top scale to the conversation. https://www.talkingmats.com/training/
TEACHING TALKING MATS Some people with communication difficulties need to learn how to do Talking Mats. Learning how to express a view can take time and has to be taught. We see pictures of what appear to be Teaching Mats. For example, starting with closed questions might be necessary to introduce the idea of preferences.
It is important that these Teaching Mats are not used as a true representation of a person’s view but seen as a step towards this skill- It can take time but great learning takes place along the way.
We have guidelines for working towards Talking Mats on our website:
Guidelines for working towards using Talking Mats – These guidelines are designed to support Talking Mats trained practitioners working with thinkers who may need to take extra steps to work towards using the Talking Mats framework
Supporting people to share what they think, and giving them the control to say when they are not happy with an aspect of their life, is within their legal rights.
‘To deny people their human rights is to challenge their very humanity’ Nelson Mandela
Many thanks to Claire Wiseman & Ann Lafferty from The Advocacy Project (Scotland) for this guest blog, including a great example of how Talking Mats helped a young woman with learning disabilities and psychosis share her views about being in hospital, receiving medical treatment and her preferences in respect of future post discharge welfare decisions:
For some time, The Advocacy Project have been thinking about how we could use the Talking Mats Framework to support people going through legislative processes such as the Mental Health (Care and Treatment) (Scotland) Act 2000, Adults with Incapacity (Scotland) Act 2000 and the Adult Support and Protection (Scotland) Act 2007.
Recently the Mental Welfare Commission published a best practice guidance on Supported Decision Making – https://www.mwcscot.org.uk/good-practice/guidance-advice, which we referred to as part of our presentation for the recent Talking Mats is 21 celebrations (click here to see the presentation Talking Mats and Supported Decision Making PP 2 (1)). The feedback from this session was that ‘yes’ there is a need for symbols to support legislation. As accredited trainers, we’ve also been asked when we’re delivering training to lawyers, Mental Health Officers, Social Workers, support workers and other advocacy organisations if there are specific symbols related to Supported Decision Making, particularly with regard to legislative issues.
Here is one of the Supported Decision Making and Talking Mats examples shared in our presentation:
One of our staff supported a young woman with a learning disability who was thought to be experiencing a psychotic episode. She had been detained in an in-patient learning disability unit under the Mental Health (Care and Treatment) (Scotland) Act 2003 on a Short Term Detention Certificate. The clinical team then made an application for a Compulsory Treatment Order, which was granted. Later, when discharge planning was in progress, an application for Welfare Guardianship was made under the Adults with Incapacity (Scotland) Act 2000.
Although the young woman was able to communicate verbally, the effects of the psychosis combined with her learning disability meant that her conversation was discursive and she was very easily distracted. Using a combination of Talking Mats and our additional symbols over a number of sessions, the advocacy worker managed to ascertain her views about being in hospital, receiving medical treatment and her preferences in respect of future post discharge welfare decisions.
The Talking Mats reports were submitted as evidence at two mental health tribunal hearings and the Welfare Guardianship hearing at the sheriff court. We received positive feedback from the Curator Ad Litem, Mental Health Officer and Sherriff regarding the reports as they had never had Talking Mats reports submitted before during these proceedings.
The use of Talking Mats had been instrumental in supporting the young woman to put forward her views and ensuring an outcome she was happy with.
Going forward, Talking Mats and The Advocacy Project will be exploring the possibility of a symbols set for Supported Decision Making and legislation. We are currently looking at funding possibilities.
A fantastic example of the power of Talking Mats – if you have any Talking Mats stories you would like to share, please get in touch! Just send me an email at laura@talkingmats.com
We are all looking forward to celebrating Talking Mats is 21 on the 15th August
The morning is aimed at people who are experienced Talking Mats practitioners and will extend thinking and Talking Mats practice. There are an interesting range of parallel sessions to choose from. Each participant will get to choose three topics to attend.
- Talking Mats as a Thinking Tool
- Embedding Talking Mats in Schools
- Talking Mats in Forensic Settings
- Talking Mats in End of Life Care
- My experience of using Talking Mats as a parent
- Talking Mats and Positive behaviour Support
- Talking Mats and Supported Decision- Making
- Empowering people with Learning Disabilities to be Talking Mats Listeners and Trainers
- Talking Mats and Children’s Mental Health
The afternoon is more informal and there will be an opportunity to engage with some of our partners – see how they use Talking Mats and try things out . There will be posters on the use of Talking Mats in lots of different places and for a wide range of applications.
Plus there will be lunch, cake and a few bubbles !
Thanks to funding from NHS Forth Valley endowment committee the event is free but you do need to book your space https://www.eventbrite.co.uk/e/talking-mats-is-21-tickets-62362171935
You can come to the morning only, afternoon only or come for the whole day.
If you can’t come to our event watch out for out blogs and social media celebrating the reach of Talking Mats for 21 days before the 15th of August .Please join in with your contributions using the hashtag #TMis21. For 21 days after our event we will be having a special Birthday offer! Watch this space, more to follow …….
We are delighted to introduce Rachel Woolcomb our first Talking Mats OT Associate. She is joining the Talking Mats Team and will be working to develop awareness and use of Talking Mats by Occupational Therapists. I will let Rachel introduce herself:
I am delighted that Talking Mats have asked me to join their team for one day a week. I am passionate about occupational therapy and about Talking Mats and to have the opportunity to bring these two loves together and seeing what develops is very exciting.
I live in South Gloucestershire and have had a varied career since I qualified as an Occupational Therapist in 1992. I was introduced to Talking Mats in 2008 and have never looked back, using them with my clients ever since.
In 2017, having spent over 25 years working in the NHS, I made the decision to move into independent practice. I work predominately with teenagers and adults who live with long term neurological conditions or who have experienced catastrophic injuries following trauma. I am very aware of the psychological impact of sudden disability and the need for people to be able to express who they are and what is important to them, even in difficult circumstances.
I now use Talking Mats with most of my clients. It doesn’t matter if they are old or young, can speak or have communication needs, they all benefit from the opportunity to stop and think and have someone really listen to them.
In the last few weeks a man who has had a stroke and has limited expressive speech has used a Talking Mat to talk about what leisure activities he used to enjoy. He then used a second mat to explain what he can and cannot achieve now. This helped us together, set goals for occupational therapy. I am also working with a teenager who has had a traumatic brain injury and now struggles with her education. She uses Talking Mats with me regularly, to think about her coping skills at school. Looking back at her previous mats is helping her to recognise progress. I have so many more examples and will be sharing them with you soon!
I really want to inspire OT’s, helping them to consider how they enable their clients to think, communicate their choices and make decisions. A Talking Mat is a great for this. It is also creative and interactive something that in my experience OT’s like! I will also be looking at important issues within the field of occupational therapy that are currently driving practice, such as personalised care, goal setting and shared decision making. I believe it is vitally important that we collaborate with our clients as together we can achieve so much more. Talking Mats is an effective tool in enabling this, so watch this space, and please do get in touch if you want to know more or have stories to share.
It is great to have Rachel working with us to build on some of the excellent work being done already in the Occupational Therapy Sector. Our Director, Lois Cameron shares why we are so excited to welcome Rachel to our Team:
‘I am really pleased that Rachel is joining us . I think the Talking Mats approach sits well with the values and approach of Occupational therapy, In my experience OTs are naturally holistic in their approach. I remember at a training course in London an OT said for her Talking Mats was the missing link in her toolkit. The training and experience of OTs allow them to see things through a different lens and that will be really helpful to us’
For more information about how OT and Talking Mats are a winning combination, take a look at Rachel’s recent blog – https://www.talkingmats.com/talking-mats-and-ot-a-winning-combination/
Feeling inspired and want to know more about the training courses we offer? See www.talkingmats.com/training/ for details.
Huge thanks to all the practitioners who have sent us guest blogs. We selected our 10 favourite guest blogs…in no particular order!
- Talking Mats to support children who stammer Kirsten Taylor, Speech and Language Therapist tells a moving story about how finding out what was upsetting a boy with a stammer helped to implement change.
- Hearing the voice of the child Emma Atkiss, Senior Educational Psychologist, shares her findings from the Wigan Pathfinder project reporting that using a Talking Mat helps to meet the 5 criteria of Shier’s model of participation.
- Talking Mats for capacity assessments in people with ASD/LD Ruth Spilman, Senior SLT from The Cambian Group, shares practical tips on assessing capacity.
- Castle hill school supports pupil voice Jenna McCammon, SLT and Rebecca Highton, SLT Assistant, tell 3 inspiring stories using TMs in: selective mutism; safeguarding and motivational interviewing.
- Supporting Looked After Children to have their say Karen Wilson, Principal Teacher for children with additional support needs in a mainstream secondary school shares her experience of using TMs to give young people a stronger voice in making decisions affecting them.
- Hearing the voices of Looked After Children Rachel Clemow, Head Teacher and Donna Wood, Education Support Worker, report that Talking Mats has enabled children to express their thoughts and views in a safe, neutral environment.
- Talking Mats and Mental Health Carla Innes, Clinical Psychologist for learning disability from Healthy Young minds Stockport talks about the impact of TM training on the whole team.
- Mummy I don’t want to go to nursery today read about how using a Talking Mat might shed some light on why a 4 year old was upset at the thought of going to nursery.
- How do you feel about starting school? The story of 4 year old twins and their thoughts about starting school.
- Sibling Attitudes Prof Juan Bornman from Pretoria in South Africa publishes a report on a study carried out with 27 typically developing children who have a younger sibling with a severe speech and language disability.
If you have been inspired and are not yet trained to use Talking Mats – come along to one of our training courses.
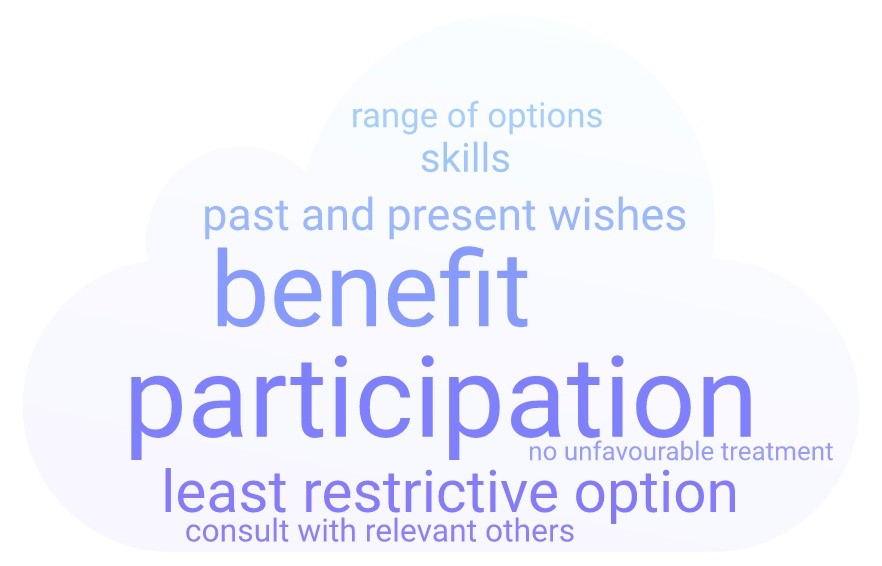
When considering someone’s mental capacity its is important to bear in mind that the right to self-determination is enshrined in law.
In 1948 Eleanor Roosevelt, as the chair of the United Nations Human Rights Commission, was the driving force in creating the Universal Declaration of Human Rights Act (1948).
Since 1948 there have been laws passed in many countries stating that people with communication disabilities should have equal rights, including and specifically in the complex area of mental capacity. In the United States the Federal Law that covers this is the Americans with Disabilities Act of 1990 . In the UK the key Acts of Parliament are the Mental Capacity Act (2005) England and Wales and the Adults with Incapacity Scotland Act (2000).
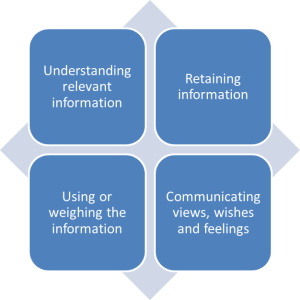
The UK Acts specifically focus on mental capacity and say that every adult has the right to make decisions unless proved otherwise and that each individual has a different capacity to make decisions about different aspects of their life. In addition they state that we must assume that someone has Capacity unless it is established that the person has substantial difficulty in one or more of the following criteria in the following diagram.
There are a number of important expectations behind these Acts which are particularly significant for people with communication difficulties.
- Everyone should be supported to make their own decisions (including Augmentative and Alternative Communication methods)
- Adults should be encouraged to make use of their skills and to learn new ones where that would be helpful
- Information to support understanding needs to be given in a way that is appropriate to his/her circumstances (using simple language, visual aids or any other means).
- People are entitled to make their decision – this is not about what we think is good or bad
- Judgements on capacity:
- cannot be based on age, behaviour or disability
- need to be made decision by decision – (so not being able to make more complicated decisions does not apply to all decisions)
- cannot be based on past experience of decisions – they need to focused on the here and now
- must take into account the adults socio-cultural circumstances wherever relevant
- where a person is able to retain the information relevant to a decision for a short period only, this should not prevent him or her from being regarded as able to make the decision
- If someone is judged to lack capacity then decisions must be in their best interest and any measures taken on their behalf are to be the least restrictive to the person
- It is important to assess people when they are in the best state to make the decision
Please let us know how you deal with self-determination and capacity issues where you work.
In a future post I will explain how Talking Mats can help support decision making and the identification of Capacity.
 Online training login
Online training login